 |
|
|
 |
IS012
Cardiac Magnetic
Resonance for the Noninvasive Diagnosis of Ischemic
Heart Disease |
|
Eike Nagel, M.D.
Cardiology-CMR
German Heart Institute
Berlin, Germany |
|
|
|
 |
|
|
 |
|
Stress cardiac magnetic resonance imaging (CMR) has tremendous
potential. This lecture focused on the use of stress CMR
for the analysis of wall motion and perfusion.
|
PAGE
TOP
|
| |
Dobutamine stress echocardiography
(DSE) is a very good method to analyze wall motion
abnormalities during stress, but in about 10-15%
of patients it is not possible to obtain adequate
image quality despite very new methods such as second
harmonic imaging. Additionally, there is a large
observer dependency for the results; much training
and practice is required to obtain reproducible
results with echocardiography (ECG). In basal lateral
and basal inferior segments there is worse image
quality and these segments can not be analyzed very
frequently.
Dobutamine stress MR (DSMR) can be
used to look at wall abnormalities at rest and at
stress. With the new imaging techniques, 5 different
views are taken: 3 short axis, a 4-chamber view,
a 2-chamber view. Complete cardiac motion of the
entire heart can be analyzed with these 5 slices
taken within 5 breath-holds of 12-15 seconds. Nagel
showed one DSMR image from the cineloop showing
the complete cardiac motion. No contrast agent was
used, as there is a very strong contrast between
the blood and myocardium can be used to visualize
motion.
Turbo gradient echo techniques or
echo planar imaging (EPI), a very new technique
that allows obtaining a complete movie of the heart
within 8-12 seconds, are now being used in their
laboratory. Real-time imaging has now been developed.
Breath-hold technique allows for using the same
stress protocols with dobutamine as with ECG. Each
step is performed within 3 minutes and then the
dobutamine dose increased to a maximum dose of 40
mcg, plus atropine as needed.
Image analysis
Image analysis is mainly done by visual
assessment, although quantitative assessment is
possible. The American Society of Echocardiography
criteria of looking at 16 segments is used, and
ischemia is defined as lack of improvement or worsening
of endocardial motion or wall thickening during
stress. One example illustrated that high doses
of dobutamine are needed to induce myocardial ischemia.
The wall motion improved from rest to 20 mcg dobutamine
but a severe wall motion abnormality was seen with
40 mcg dobutamine stress.
To perform an analysis it is best
to view all the stress levels simultaneously. This
can be done in a quad-screen format as in ECG showing
the images only at rest, or using a newly developed
tool by Hundley to show all different stress levels
simultaneously. The studies of dobutamine stress
for the diagnosis of ischemia performed through
1999 used a maximum dobutamine dose of 20 mcg, as
the gradient techniques allowing an image to be
obtained within one breath-hold was not available.
The ability now to use high dobutamine stress has
increased the sensitivity and specificity of DSMR
imaging to about 85%, improving diagnostic accuracy.
|
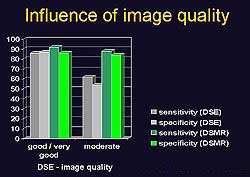 |
Figure
1. A comparison of moderate echocardiographic
image quality obtained with dobutamine stress
echocardiography (DSE) to images obtained with
dobutamine stress magenetic resonance (DSMR) imaging
shows a statistically significant difference in
terms of sensitivity and specificity. (Z. Cardiol
1999;88(9):622-630.)
Click to
enlarge |
|
Influence of image quality
A comparison of moderate echocardiographic
image quality obtained with DSE to images obtained
with DSMR shows a statistically significant difference
in terms of sensitivity (62% vs 90%, respectively)
and specificity (55% vs 82%) [Fig. 1]. Comparing
good and very good image quality obtained with DSE
to DSMR there is little difference in sensitivity
and specificity, all at about 90%. However, even
with second harmonic imaging, good or very good
images were only obtained in about 50% of patients
with DSE. Therefore, in about 50% of patients much
better diagnosis can be obtained with DSMR than
with DSE.
Limitations of DSMR
Patients with claustrophobia or metallic
implants (pacemaker, implantable cardioverters)
can not be examined. This problem may be solved
with new pacemaker techniques. The problem of reduced
image quality in patients with frequent premature
ventricular complex or atrial fibrillation has been
addressed using the breath-hold technique and the
images are re-constructed within a few seconds after
acquisition, which might be a safety problem. However,
real-time techniques may be useful, requiring about
55-60 ms to acquire one image. ECG triggering is
not required. The real-time images compare well
with those obtained with turbo field echo (TFE)
or EPI, with wall thickening, wall motion, and endocardial
motion assessable. Real-time DSMR has been shown
to capture 97% of the wall abnormalities seen with
the standard technique.
Steady state technique
These images do not require inflow
contrast, whereas standard techniques are dependent
on fresh blood inflow, providing a 3-fold increase
in contrast between the blood and myocardium in
contrast to standard technique. This is advantageous
in patients with low ejection fraction or for long
axis views.
|
|
PAGE
TOP
|
| |
At the onset of ischemia a perfusion
deficit is seen, and later in the course wall motion
abnormalities, ECG changes and anginal pain are
seen. Wall motion abnormalities are in principle
less sensitive than looking at perfusion defect
itself. Problems with the techniques routinely used,
positron emission tomography (PET) and single-photon
emission computed tomography (SPECT), include low
spatial resolution, attenuation artifacts, and radiation.
MR is highly promising technique for assessing myocardial
perfusion, based on preliminary study results. One
example showed that not only could perfusion be
assessed, but that the defect was subendocardial,
not transmural, which would not have been seen with
nuclear techniques.
Five to seven short-axis views
per heart beat are acquired--an important improvement
in ability. A contrast injection is given which
goes first into the right ventricle and then the
left ventricle and then into myocardium.
|
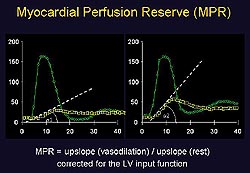 |
Figure
2. An alteration of the upslope can be obtained
if the contrast is given before or after vasodilation
with adenosine or dipyridamole. (Nagel 2000)
Click to
enlarge |
|
An alteration of the upslope can
be obtained if the contrast is given before or after
vasodilation with adenosine or dipyridamole (Fig.
2). This is done for 6 segments per slice, for a total
of 30 segments per patient. This technique has been
validated in a highly selected group of patients with
high-grade proximal single vessel stenoses. A good
differentiation between segments supplied by high-grade
stenotic coronary artery and control segments was
used. From this study they developed a cut-off value
of 1.5 MP/L which was then used for a prospective
study. They have also shown that the upslope parameter
is highly reproducible.
The recent studies of detection of
coronary disease with MR have sensitivity (90-92%)
and specificity (84-87%) rates comparable to those
with nuclear imaging. A further development is the
intravascular contrast agents that may further refine
this technique. Current contrast agents show both
perfusion and diffusion as the contrast agent moves
from the vascular to the interstitial space during
the first pass.
|
|
PAGE
TOP
|
MR stress studies are possible today that can be
used routinely for the detection of wall motion
abnormalities that are much better than echocardiography,
particularly if the echo images are suboptimal.
MR perfusion studies can be done routinely with
results that are highly promising and better than
those with nuclear medicine. Wall motion and perfusion
studies during stress can be combined into a single
stress test, allowing CMR to be used routinely.
|
|
PAGE
TOP
|
At his institution, a 35 ms temporary
resolution is used to ensure that end systolic images
are not missed. A time of 15 ms might be too short
to observe relaxation disturbances such as early
diastolic filling; better resolution is required,
which is possible by either increasing measurement
time or reducing spatial resolution. In response
to a question about intrinsic motion of infarcted
areas, Nagel stated that can not be done with normal
wall motion analysis because passive movement can
not be discerned as well from actively moving areas.
However, there are two criteria that help. One,
wall thickening itself because there is good contrast
between the blood and endocardium with MR and also
between the epicardium and fat allowing good visualization
of wall thickening. This helps to discern passively
moving areas that are just pulled towards the center
versus actively contracting areas that thicken by
themselves. Two, myocardial tagging that shows intrinsic
shortening can be used.
Commenting on whether wall imaging
during dobutamine or perfusion imaging during vasodilation
is easiest to use today considering both acquisition
and post-processing, Nagel stated there was no definite
answer. In his institution it is currently easier
to perform wall motion analysis due to their large
experience with dobutamine. If one begins to do
stress studies, one may select not to do high dose
dobutamine studies in the MR scanner as some experience
is needed. The stress study itself is easier with
adenosine or dipyridamole. However, because post-processing
is much more difficult for the perfusion imaging
very good software is needed for the analysis, and
this is not yet routinely available.
|
|
PAGE
TOP
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2000
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|