|
Based on his studies of echocardiography and molecular
and cellular biology, Kitabatake shared his views
on the recent progress in research of heart failure
and the prospect for its treatment.
Traditionally heart failure has been defined
as a clinical syndrome resulting from the inability
of the heart to pump sufficient blood to supply the
metabolic needs of the body. Left ventricular (LV)
systolic dysfunction has been considered to play a
major role in heart failure. However, epidemiological
studies suggest that 20-40% of patients with heart
failure have preserved systolic function. Diastolic
function was of little concern twenty years ago because
of its difficult evaluation. Work by Kitabatake in
the 1970s showed that physiological properties of
the papillary muscle in situ might be affected by
coronary perfusion pressure. That is, the systemic
environment affects the mechanical properties of the
left ventricle. Further work in the animal model showed
that the ejection timing, rather than peak LV pressure,
was the primary determinant of the LV relaxation rate.
|
|
Assessment of Diastolic Function |
|
Work by Kitabatake and colleagues showed that measurement
of the transmitral flow pattern (E/A ratio) is feasible
but pseudo-normalized, and that the flow propagation
velocity (FPV) is much more useful to non-invasively
evaluate LV diastolic function in humans and is not
pseudo-normalized, even in patients with severe heart
failure. FPV closely correlates with Tau, exercise
capacity and prognosis in patients with impaired systolic
function.
A new ultrasound system combining pulse Doppler technique
and two-dimensional echocardiography to non-invasively
evaluate LV diastolic properties in humans was developed
by Kitabatake and colleagues. The direction of the
pulse Doppler flow meter with an electronic beam sector
scanning echocardiograph enabled the precise location
of the sample volume of the Doppler beam on 2-D echocardiogram.
Regional blood flow evaluation is possible anywhere
in the cardiovascular system with this system, as
is non-invasive assessment of pulmonary arterial pressure.
Accurate measurement of transmitral blood flow velocity,
shown to reflect the diastolic behavior of the left
ventricle in health and disease, is also possible.
Throughout the diastolic period, the area of the
mitral valve orifice remains nearly unchanged, so
the transmitral velocity flow pattern reflects LV
volume changes essentially equivalent to the dv/dt
curve in diastole. Thus, Doppler measurement may allow
the estimation of sequential LV volume changes without
invasive scintigraphy.
By the mid-1980s, a consensus was achieved that LV
diastolic function might decrease E wave amplitude
because of incompetent early relaxation of the ventricle
and increased A wave amplitude because of compensatory
atrial contraction, resulting in a decrease in the
E/A ratio. Pseudo-normalization of the transmitral
flow pattern in patients with dilated cardiomyopathy
(DCM), in which in the absence of heart failure the
E wave amplitude and the E/A ratio is decreased to
less than 1.0, while in the presence of severe heart
failure the E wave amplitude and E/A ratio increased,
was identified by Kitabatake and colleagues. The peak
systolic to diastolic flow velocity ratio (S/D) in
primary venous flow allows differentiation of pseudo-normalized
from normal transmitral flow pattern. However, this
method was somewhat complicated.
Color M-mode Doppler echocardiography was then studied
to improve clinical evaluation of LV diastolic function.
The flow propagation velocity (FPV) as a new diastolic
index was defined as the ratio between the maximal
velocity around the mitral orifice (Lmax) in early
diastole and the decrease to 70% of the maximal velocity
(L70). FPV is not pseudo-normalized, making
it a useful index for evaluating LV relaxation, even
in patients with severe heart failure. Hence, evaluation
of LV diastolic function, regardless of heart failure
severity, was made possible.
Diastolic function is a major determinant of exercise
capacity, as shown by the significant correlation
between peak VO2 and FPV on color M-mode
Doppler echocardiography. Peak VO2 as an
index of exercise capacity did not correlate with
ejection fraction as determined by 2-D echocardiogram.
Cumulative event-free survival was significantly better
in the mild diastolic dysfunction than in the severe
dysfunction group. This finding strongly indicated
that the degree of diastolic dysfunction of the ventricle
is relevant to the prognosis in patients with impaired
systolic function.
|
PAGE
TOP
|
Molecular Signaling in Heart Failure |
|
Neurohormonal activation worsens the natural history
of myocardial dysfunction and remodeling. In essence,
multiple neurohormonal signaling pathways such as
alpha-1 and angiotensin II type-1 receptors are activated
in the failing heart and promote maladaptive remodeling
and myocardial dysfunction. Improved understanding
of the molecular biology and mechanisms of the signal
transduction system would improve the understanding
of cardiac performance.
The BIO TO2 strain of the cardiomyopathic hamster
is an animal model of DCM and heart failure. At 20
weeks in this model, LV diastolic dimension was significantly
higher and the percent fractional shortening (%FS)
was significantly lower. At 26 weeks, the ventricular
wall was thinner and the left ventricle more dilated
than in the control animal. Interstitial fibrosis
could also be seen in the BIO TO2 animals, with increased
interstitial space. The decreased nuclear density
in the BIO TO2 animal was closely correlated with
%FS, demonstrating that cardiac dysfunction is accompanied
by a loss of cardiomyocytes. Total collagen content
increased with age in the BIO TO2 animals while it
remained the same in the control animals, and the
difference was significant at 10-20 weeks of age.
As total collagen content increased, the %FS decreased
more. These findings indicate that an increase in
collagen content might be due to LV dysfunction.
|
PAGE
TOP
|
PI Signaling in Remodeling Myocardium |
|
Expression of mRNA of angiotensinogen, renin, and
ACE was about 2-fold higher in the left ventricle
of spontaneously hypertensive rats (SHR) than in Wistar
Kyoto rats (WKR), suggesting that the tissue angiotensin
II formation pathway was enhanced in the hypertrophied
remodeled heart, as in the failing heart of the BIO
TO2 animals.
In LV hypertrophy (LVH), extracellular matrix protein,
collagen and cardiomyocytes are major components of
the LV wall. The effects of angiotensin II on collagen
synthesis in cardiofibroblasts isolated from SHR and
WKR was studied. A 2-fold increase in collagen synthesis
resulted from 2-hours of angiotensin II stimulation
of cardiofibroblasts, which was completely inhibited
by the angiotensin II type-1 antagonist MK954, but
not by the type-2 antagonist PD123177. Thus, in the
remodeled myocardium of SHR, tissue expression of
the components of the renin angiotensin system (RAS)
is increased. This cardiac RAS activation may cause
myocardial fibrosis by stimulating collagen synthesis.
Phosphatidyl inositol (PI) metabolism during the
cellular response to norepinephrine in the pressure
overloaded hypertrophic rat heart was examined in
SHR. The calcium influx stimulated by norepinephrine
was higher in SHR and the release of DAG from cardiomyocytes
was markedly increased. The accumulation of IP3 significantly
increased, indicating that PI-specific PLC activity
increased in SHR. PLC activity was also enhanced in
SHR. Thus, in the remodeled myocardium, the cytosolic
calcium concentration may increase in response to
stimuli such as angiotensin II or endothelin, whose
receptors are coupled to Gq proteins, like norepinephrine.
|
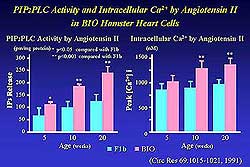 |
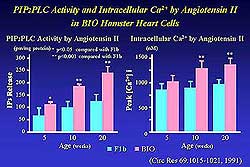
| Figure
1. The effect of angiotensin II on PIP2PLC activity
as measured by IP3 release and intracellular Ca2+
in BIO hamster heart cells. |
| Click
to enlarge |
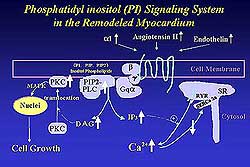 |
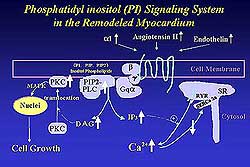
| Figure
2. Schematic of the phosphatidyl inositol system
in remodeled myocardium. |
| Click
to enlarge |
|
Enhanced cardiac RAS may increase IP3 and DAG production
in cardiomyocytes in BIO TO2 animals. In fact, IP3
release was markedly increased by angiotensin II and
the intracellular calcium concentration was higher
in BIO animals from 5 to 20 weeks of age (Figure 1).
These findings suggest that angiotensin formation
via ACE was increased and the angiotensin II signaling
and the PI turnover might produce a higher intracellular
calcium level in the BIO TO2 animals. These changes
in PI turnover are essentially similar in hypertrophied
or failing myocardium.
PI signaling was altered in isolated cardiomyocytes
from SHR and BIO TO2 animals. Activated PIP2-PLC resulted
in increases in secondary messengers such as IP3 and
DAG, which induced translocation of PKC from cytosol
to the plasma membrane leading to activation of the
MAP-kinase cascade. The PI turnover pathway may play
an important role in the remodeling process. Figure
2 illustrates the PI signaling system in remodeled
myocardium. Receptor-mediated activation of myocardial
Gq signaling is a biochemical mechanism postulated
to be responsible for inducing pressure overload hypertrophy.
Serial echocardiographic findings in Gq-transgenic
mice and non-transgenic mice show that the LV is more
dilated and wall motion is decreased after aortic
banding in the mice overexpressing myocardial Gq.
The LV mass of both species increased after aortic
banding. The %FS progressively declined after aortic
banding in the Gq-transgenic mice, while it was preserved
in the non-transgenic mice. Gq-stimulated cardiac
hypertrophy is functionally deleterious and compromises
the ability of the heart to adapt to an increased
mechanical load. The hypertrophic response to receptor-mediated
signaling might differ from that in Gq-stimulated
signaling, implying that physiological stimuli are
regulated by integrated crosstalk with other signal
transduction systems.
|
PAGE
TOP
|
Beta-adrenergic Receptor Signaling in Heart Failure |
|
Heart failure is associated with a diminished contractile
response to catecholamines. In contrast to the redundancy
associated with the Gq-coupled receptor signaling,
the number of beta-adrenergic receptors and the agonist-stimulated
adenyl cyclase (AC) activity is reduced in the failing
myocardium.
Forskolin-stimulated AC activity was markedly decreased
at the age of 16 and 28 weeks. G-protein coupled receptor
kinases (GRKS) are known for their agonist-dependent
phosphorylation of beta-adrenergic receptors. Semi-quantitative
RTPCR revealed that expression of GRK2 and GRK5 was
significantly higher in the BIO TO2 than in the F1b
animals. It has been demonstrated that gene targeting
of GRKs directly affects the cardiac function. Taken
together with the findings by Kitabatake, it is likely
that GRKs might be one of the responsible factors
for reducing cardiac contractility.
A new molecule, rap1GAPII, was found to be a Gi-associated
isoform of rap1GAP. The association of Gi and rap1GAPII
resulted in the activation of ERK MAP-kinase by inactivating
rap1. An agonist dependent decrease in GTPrap1 occurred
with co- transfection of M2 muscarinic-receptors.
These results suggested that M2-dependent Gi activation
may cause GTPrap1 hydrolysis attributed to the activation
of rap1GAPII. Mice overexpressing rap1GAPII in the
heart are now being developed by Kitabatake and colleagues.
|
PAGE
TOP
|
Clinical
Significance of Altered Transduction Signaling |
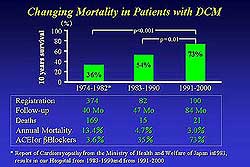 |
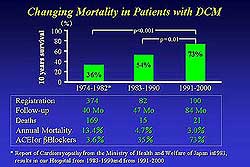
| Figure
3. The 10-year survival rate in three cohort studies
of patients with dilated cardiomyopathy and the
percentage of patients receiving beta blocker
and ACE inhibitor therapy. |
| Click
to enlarge |
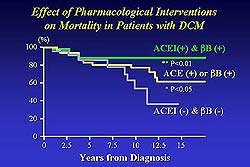 |
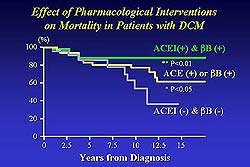
| Figure
4. The improved prognosis for patients with dilated
cardiomyopathy receiving both beta blocker and
ACE inhibitor therapy compared to those patients
who are not. |
| Click
to enlarge |
|
Three cohort
studies corresponding to three different periods, each
8-10 years, were compared to investigate the changes
in mortality in patients with DCM in the past 30 years
and identify factors that might have influenced survival.
Patients in Group I were enrolled between 1974 and 1982
in 17 centers in Japan. Group II patients were enrolled
between 1983 and 1990 in Japan, while Group III patients
were enrolled between 1991 and 2000 in Hokkaido University
Hospital. The 10-year survival rate was 36% in Group
I, 54% in Group II and 73% in Group III (Figure 3).
Only 3.6% of patients in Group I were treated with ACE
inhibitors or beta blockers, while in Groups II and
III 35% and 73%, respectively, received these drugs.
Pharmacological treatment, particularly with ACE inhibitors
and beta blockers, has improved the prognosis of DCM
(Figure 4). |
PAGE
TOP
|
| For the measurement
of diastolic function, changes in regional blood flow
as a result of organ function provides a key to evaluate
cardiovascular function. Analytical and molecular approaches
to heart failure reveal that altered signal transduction
could be identified in cells of the remodeled myocardium.
These findings have led to the use of ACE inhibitors,
which suppress activation of RAS, thereby providing
one of the modern therapeutic approaches to heart failure.
Beta blockers offer a similar therapeutic strategy.
However, studying each element alone will not achieve
the goal of preventing and treating heart failure. Therefore,
constitutive approaches are needed to understand how
to efficiently reconstitute and reintegrate the various
elements (gene, cell, tissue, organ, system, human)
taking full advantage of the knowledge at the micro
and macro levels. |
PAGE
TOP
|
Report
Index | Previous Report | Next
Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2002
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|