Two-dimensional speckle tracking (2-D ST) and tissue Doppler imaging (TDI), recent advances in echocardiography that allow non-invasive assessment of regional myocardial motion, were used in two studies by Tanimoto and colleagues at Wakayama Medical University presented in this lecture. The results of these studies showed these new modalities are useful non-invasive methods to assess myocardial ischemia and the transmural extent of myocardial necrosis in patients with angina pectoris and myocardial infarction.
Assessment of baseline parameters
|
Figure 1. A representative normal subject who had tissue strain imaging. In the color-coded strain image obtained by TDI-Q (left panel) the bright color indicates the myocardial thickening. The brighter endocardial layer compared to the epicardial layer indicates the heterogeneous wall thickening. The brighter endocardial layer compared to the epicardial layer indicates the heterogeneous wall thickening.
【Click to enlarge】 |
|
|
|
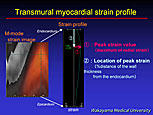
Figure 2. Transmural myocardial strain profile in a normal subject at end systole shows the strain is highest at the subendocardial side and liner regression to the epicardium is seen (middle panel). Peak strain was calculated as the percent of the distance of the wall thickness from the endocardium (right panel).
【Click to enlarge】 |
|
|
Regional systolic function was evaluated in 15 patients with angina pectoris and 30 patients with ST segment elevation acute myocardial infarction (AMI) before the studies in these two groups. The commercially available ultrasound machines and analytical software used automatically divided the left ventricle (LV) into six segments, allowing assessment of radius, circumferential strain, and rotation in each segment.
Figure 1 illustrates the images obtained with the tissue strain imaging technique.
In this representative normal subject, the color-coded strain image obtained by TDI-Q is shown in the left panel, with myocardial thickening indicated by the bright color. M-mode strain images are obtained by placing the M-mode cursor at left ventricle. Heterogeneity of wall thickening is indicated by the brighter endocardial layer compared to the epicardial layer.
Figure 2 illustrates the transmural myocardial strain profile at end systole (middle panel). The strain is highest at the subendocardial side and shows a liner regression to the epicardium in a normal subject. Peak strain value, which indicates the highest radial strain of the ventricular wall, was measured, and the location of the peak strain value was calculated as the percent of the distance of the wall thickness from the endocardium.
Study of angina pectoris
Tanimoto and colleagues adapted these techniques to study the 15 patients with angina pectoris undergoing percutaneous coronary intervention (PCI). LV wall motion was recorded during PCI and Echo during and after balloon occlusion. The asynergy of the antero-septal wall was easily detected during the 15-second balloon occlusion, and improvement of asynergy was seen after balloon deflation.
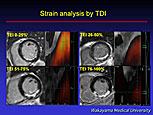
In a representative case of angina analyzed by TDI, during ischemia the location of peak strain shifted from the subendocardial to the epicardial side, and this shift improved after balloon deflation. At baseline the peak strain value was 0.67 compared to 0.48 during ischemia and 0.74 during recovery. The location of peak strain was 11.3 at baseline and 47.4 during ischemia, and 15.4 during recovery.
In these patients, TDI assessment after 15-second balloon occlusion showed the peak strain value significantly decreased to 0.43 (from 1.12 at baseline) and significantly improved at the recovery phase to 0.96. During balloon occlusion, the location of peak strain significantly shifted from the endocardial to epicardial side, and returned to the endocardial side during the recovery phase. The 2-D ST during and after balloon occlusion revealed that the rotation decreased and that it improved more rapidly than did the radial or the circumferential strain.
Study of AMI
In the 30 patients with AMI, echocardiography was performed twice within the first 24-hours and 2 weeks after AMI onset to record LV wall motion. Cardiac MRI to assess the extent of myocardial necrosis was performed. Patients with an unsuccessful PCI, atrial fibrillation, renal dysfunction, or contraindications to MRI were excluded.
|
Figure 3. MRI and strain images of patients with inferior MI revealed that the location of peak strain shifted from the endocardial to epicardial side as the necrosis extends more deeply
【Click to enlarge】 |
|
|
Transmural extent of infarction (TEI) was obtained by MRI two weeks after MI onset, and patients were divided into 4 groups. MRI and strain images of patients with inferior MI revealed that the location of peak strain shifted from the endocardial to epicardial side as the necrosis extended more deeply (Figure 3). Further, as the TEI increased, peak strain value decreased and the location of the peak strain shifted from the endocardial to epicardial side.
Combining a cut-off value of 43 for peak strain value and 58 for location of peak strain provided a sensitivity of 100% and specificity of 97% for predicting non-viable myocardial muscle.
Regarding 2-D ST, they found that the recovery of rotation is lower as the TEI increased, and similar results were found for radial and circumferential strain, when comparing the acute and subacute phases. |