|
|
ACC-JCS Joint Symposium |
| |
| Optimal Strategy for Cardiac Resynchronization Therapy: Who Can Benefit From CRT? |
|
| |
|
| The Japanese Experiences for the Detection of the CRT Non-Responders and the Benefits of Triangle Ventricular Pacing. |
| Kazutaka Aonuma |
| Division of Cardiovascular Science, Graduate School of Comprehensive Human Sciences, University of Tsukuba, Japan |
| |
Dr. Kazutaka Aonuma, University of Tsukuba, Japan, presented the results of the Japanese CRT (J-CRT) study and studies of triangle ventricular (Tri-V) pacing hemodynamic performance. The objective of the J-CRT prospective multicenter study was to identify echocardiographic dyssynchrony parameters for predicting response to CRT. A total of 209 patients from the J-CRT Registry with heart failure (HF) refractory to medical therapy, NYHA class III/IV, left ventricular ejection fraction (LVEF) ≤35%, and QRS duration ≥130 ms were evaluated.
Echocardiographic dyssynchrony parameters evaluated included: Intraventricular dyssynchrony–septal-to-posterior wall motion delay (SPWMD), Ts (lateral-septal); interventricular dyssynchrony–interventricular mechanical delay (IMD), LV pre-ejection period (LV-PEP); and atrio-ventricular dyssynchrony–LV diastolic filling time (DFT/RR). The primary endpoint for CRT response was a ≥15% reduction in left ventricular end-systolic volume (LVEDV).
After 6 months follow-up, 121 (58%) patients responded to CRT responders and 88 (42%) did not respond. There were significantly more hospital readmissions for HF (p=0.0010), more deaths from HF (p=0.0044), and more deaths from any cause (p=0.0006) among nonresponders than responders. Dyssynchrony parameters that were worse in nonresponders versus responders were SPWMD (p=0.008), Ts (lateral-septal) (p=0.002) and IMD (p=0.008). There was no difference in QRS duration AUC between the two groups. The difference in SPWMD and IMD AUC between responders and nonresponders was not enough to predict nonresponse.
In this study, no single echocardiographic dyssynchrony parameter was adequate to identify CRT responders. Multifactorial evaluations including intraventricular, interventricular, and atrio-ventricular dyssynchrony parameters are needed to predict true CRT responders.
Conventional bi-ventricular (Bi-V) pacing is associated with a 30%-40% nonresponse rate. Dr. Aonuma et al invented Tri-V pacing to improve response rates. Tri-V pacing paces the left ventricle, right ventricular apex (RVAP), and RV outflow tract (RVOT). Comparison of CRT with Bi-V and Tri-V pacing showed that dyssynchrony still existed with Bi-V pacing, while resynchronization had greater improvement with Tri-V pacing. Tri-V pacing produced greater improvements in dp/dt max (p=0.002), tau (p=0.002), and Ts-SD (p=0.02) versus Bi-V pacing. There also were improvements in systolic pressure, cardiac output, and pulmonary capillary wedge pressure (PCWP) with Tri-V pacing. Tri-V CRT pacing improved the antero-lateral motion to a greater extent than Bi-V pacing.
In these studies, Tri-V pacing provided better hemodynamic performance than Bi-V pacing. Echocardiographic dyssynchrony parameters were significantly improved with Tri-V versus Bi-V CRT pacing. Implantation of a Tri-V pacing device appears to hold promise for patients with end-stage heart failure. |
| |
| Page Top |
|
| |
|
| Novel Cardiac Imaging to Quantify Dyssynchrony and to Predict Response to CRT–Overview. |
| Satoshi Nakatani |
| Osaka University Graduate School of Medicine, Osaka, Japan |
| |
|
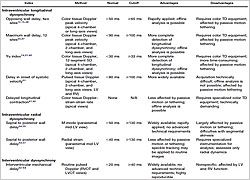
Figure 1. Echocardiographic parameters for evaluating dyssynchrony.
【Click to enlarge】 |
|
|
Dr. Satoshi Nakatani, Osaka University Graduate School of Medicine, reviewed imaging methods to assess dyssynchrony for distinguishing CRT responders from nonresponders. Several echocardiographic parameters have been developed for evaluating dyssynchrony (Figure 1). The PROSPECT trial evaluated 12 echocardiographic parameters of dyssynchrony and found large variability in analysis of the parameters, concluding that no single measure of dyssynchrony could be recommended for improving patient selection for CRT.
The 2008 ASE Expert Consensus Statement on echocardiography for CRT recommended that in patients meeting standard criteria for CRT, CRT should not be withheld because of echocardiographic Doppler dyssynchrony results. The statement recommended that dyssynchrony reports should not include recommendations for or against CRT and that the decision should be made on a case-by-case basis. The statement acknowledged that some new methods have the potential to impact future clinical practice.
Myocardial strain might be a potential method for evaluating dyssynchrony. Myocardial strain is an index of tissue deformation (∆L/L) that can be measured by tissue velocity imaging (TVI) or speckle tracking. The Mayo Clinic reported that TVI-based strain is better than TVI. One report comparing TVI and strain parameters in 45 patients with systolic heart failure (HF) found that the strain dyssynchrony index (standard deviation of time to peak strain) is a better measure than TVI parameters for predicting LV volume reduction after CRT (p<0.001). Another Mayo study compared TVI and strain parameters in 120 subjects, concluding that a substantial proportion of normal subjects have abnormal TVI parameters and that the strain parameter is more specific for dyssynchrony.
|
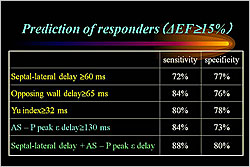
Figure 2. Prediction of responders.
【Click to enlarge】 |
|
|
Suffoletto et al reported that speckle tracking radial strain can quantify dyssynchrony and predict immediate and long-term response to CRT. The time difference in peak septal wall-to-posterior wall strain ≥130 ms predicted LV remodeling after CRT. Gorcsan et al reported that combined longitudinal and radial dyssynchrony predicts ventricular response after CRT. This combination provided the best sensitivity (88%) and specificity (80%) for predicting LV improvement after CRT (Figure 2). Another study found that a cut-off of radial dyssynchrony ≥130 ms predicted response to CRT with 83% sensitivity and 80% specificity. A Cleveland Clinic group reported that longitudinal strain delay index by speckle tracking is a new marker of response to CRT.
Dr. Nakatani concluded that tissue velocity is easy and simple but is susceptible to noise and has unsatisfactory reproducibility. Strain is more robust than tissue velocity for predicting response to CRT. |
| |
| Page Top |
|
| |
|
| CRT for Patients with AF |
| Morio Shoda |
Department of Cardiology, Tokyo Women’s Medical University, Tokyo, Japan |
| |
Dr. Morio Shoda, Tokyo Women’s Medical University, reviewed studies of cardiac resynchronization therapy (CRT) in heart failure (HF) patients with atrial fibrillation (AF). The prevalence of AF in HF patients is high, ranging from 4.2% in NYHA class I patients to 49.8% in NYHA class IV patients. Although the efficacy of CRT in patients with sinus rhythm (SR) has been established, the ACC/AHA 2008 HF guidelines only recommend CRT for patients with AF as a class IIa indication. Patients with AF are at a disadvantage because atrio-ventricular (AV) timing can’t be resynchronized with CRT.
The MILOS non-randomized observational study evaluated CRT in 1,042 patients with SR and 243 patients with AF. At 72 months follow-up, there were no significant differences in overall, cardiac, and HF survival between the SR and AF patients. Another long-term observational study found that CRT was equally effective in improving NYHA class, 6-minute walk distance (6MWD), and QoL score in SR (N=209) and AF (N=86) patients. LVEDV, LVESV, and EF were similarly improved in both groups. Mortality rates in the SR and AF groups were similar.
A meta-analysis of five prospective cohort studies found the relative risk of all-cause mortality favored AF patients versus SR patients receiving CRT (RR=1.57, 95% CI 0.87, 2.81). The change in EF also favored AF over SR patients (p<0.00001). However SR patients had better results with respect to change in NYHA class (p<0.00001), 6MWD (p<0.00001), and QRS score (p<0.00001).
A recent study showed that a 100% biventricular (BiV) pacing rate is associated with lower HF hospitalization and all-cause mortality than lower rates. The BiV pacing rate can be increased in AF patients with drugs or AV junction ablation (AVJ-abl). In the MILO study comparing long-term survival after CRT, AF patients treated with AVJ-abl had significantly better overall (p=0.010), cardiac (p=0.048), and HF (p=0.016) survival versus AF patients treated with drugs. However, AVJ-abl has several limitations.
|
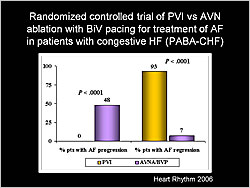
Figure 1. Randomized controlled trial of PVI vs AVN ablation with biventricular pacing for treatment of AF in patients with congestive HF (PABA-CHF).
【Click to enlarge】 |
|
|
A randomized trial in HF patients with AF found that pulmonary vein isolation (PVI) was more effective than AV node (AVN) ablation with BiV pacing for preventing AF progression (p<0.0001) and causing AF regression (p<0.0001) (Figure 1).
Dr. Shoda concluded that CRT can be effective for patients with HF, LV dyssynchrony, and AF. Rate control is important for maximal CRT response. Properly designed randomized trials are necessary to clarify the role of AV nodal ablation in patients with chronic AF receiving CRT.
|
| |
| Page Top |
|
| |
|
Emerging Indications for Cardiac Resynchronization Therapy. |
| John F. Beshai |
| University of Chicago, Chicago, Illinois, USA |
| |
Dr. John F. Beshai, University of Chicago, reviewed trials of cardiac resynchronization therapy (CRT) in different patient populations. The Miracle ICD II (N=186) and CONTAK CD (N=248) trials found no difference in exercise capacity at 6 months in patients with NYHA class I/II heart failure (HF) who received CRT versus no CRT. In the MIRACLE ICD II trial, left ventricular ejection fraction (LVEF), LV end diastolic volume (EDV), and LV end systolic volume (ESV) improved with CRT. In the CONTAK CD trial, LVEF was not improved but LV systolic and diastolic dimensions were improved with CRT.
The REVERSE trial (N=610, NYHA I/II) found that the pre-specified clinical composite response at 12 months was not significantly different with CRT versus no CRT. Conventional analysis showed that more CRT patients (54%) improved versus no-CRT patients (40%) (p=0.004). LVESV, LVEDV, and LVEF improved with CRT versus no CRT (p<0.0001). Time to first HF hospitalization was reduced with CRT versus no CRT (p=0.03).
About 30% of HF patients have left bundle branch block (LBBB), of which 50% qualify for CRT and 70% of those are responders. Thus, only 9% of the total HF population benefit from CRT. If the pool of patients who qualify for CRT could be expanded to those with narrow QRS and mechanical dyssynchrony, more patients might benefit. A small study of CRT in patients with narrow QRS (N=33) and LV dyssynchrony ≥65 ms found significant improvements in QoL-score, 6-minute walk test, LVEF, and LVESV.
The RETHINQ trial in patients with NYHA class III HF with narrow QRS (<130 ms) and mechanical dyssynchrony found no difference at 6 months in peak oxygen consumption and peak V02 in patients who received CRT versus controls. Patients with QRS ≥120 ms did have improved peak V02 with CRT versus no CRT (p=0.02). There were no improvements in other objective parameters but NYHA class did improve with CRT.
Dr. Beshai concluded that CRT is a proven effective therapy in patients with wide QRS, EF ≤35%, and NYA class III/IV HF. CRT may benefit certain patients with atrial fibrillation and prevent disease progression in patients with NYHA I/II HF. Clinical trials evaluating CRT in these populations are ongoing. While smaller single center trials have demonstrated benefit of CRT in narrow QRS with evidence of mechanical dyssynchrony, a large scale randomized trial did not. Better methods for identifying mechanical dyssynchrony and potential responders need to be evaluated further.
|
| |
| Page Top |
|
| |
|
|