Dr. Albert A. Hagege, Hopital Europeen G. Pompidou, reviewed studies of atrial fibrillation (AF) in patients with hypertrophic cardiomyopathy (HCM). The prevalence of AF in patients with HCM ranges from 10-22%. The incidence of embolic events in non-selected patients with HCM is 0.8% annually. Multivariate analysis showed that the main risk factors for AF in HCM patients were age >50 years (OR=2.3, p<0.001), NYHA class III/IV (OR=2.8, p<0.005), and left atrial (LA) dimension ≥45 mm (OR=3.4, p<0.0001). More than 30% of patients with LA >45 mm and NYHA class II-IV develop AF by 6 years (p<0.0001). P wave duration ≥140 ms plus LA >40 mm also predicts AF in HCM patients.
|
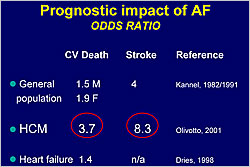
Figure 1. Prognostic impact of atrial fibrillation.
【Click to enlarge】 |
|
|
|
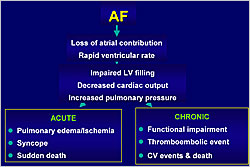
Figure 2. Morbidity and mortality associated with atrial fibrillation.
【Click to enlarge】 |
|
|
HCM patients with AF have a higher risk for CV death (OR=3.7) and stroke (OR=8.3) than the general population and patients with heart failure (HF) (Figure 1). AF can lead to pulmonary edema/ischemia, syncope, and sudden death in the acute setting and to functional impairment, thromboembolic events, and death in the chronic setting (Figure 2). HCM patients with AF have higher risk of mortality (p<0.0001) and cumulative risk of embolism (p<0.0001) than those with SR. The probability of HCM-related adverse outcomes is higher with chronic versus paroxysmal AF (p<0.0001).
More HCM patients with vascular events have NYHA class III/IV (p<0.005), history of AF (p<0.001), LA dimension ≥45 ms (p<0.001), and age >60 years (p<0.01). HCM patients with AF and outflow obstruction have a higher risk of death than those with AF without obstruction (p<0.0001). Patients ≤50 years with AF have higher rates of mortality (p<0.001), stroke (p<0.0001), and progression to NYHA III/IV (p<0.0001) than those >50 years.
Patients with HCM and AF are treated with anticoagulation and rate control or rhythm control therapies. Olivotto showed that HCM patients with chronic AF over time had a higher probability of CV death, embolism, and/or progression to NYHA class III/IV versus those maintained in SR (p<0.001).
AF is the most common sustained arrhythmia in patients with HCM. The main risk factors are LA dilatation, advanced age, and NYHA class. AF is associated with disease progression, a 4-fold increase in mortality, and 8-fold increase in embolic events. Early onset and obstruction markedly increase the risk of adverse outcomes. Maintenance of SR is associated with better outcomes. Long-term anticoagulation is necessary once paroxysmal or chronic AF occurs. As stroke may be the first manifestation of AF, progressive LA dilatation is an indication for repeat Holter ECG and consideration of anticoagulation.
|