|
|
Plenary Session 4 |
| |
| Pathophysiology and Therapeutic Strategy for Diastolic Dysfunction in Heart Failure. |
|
| |
|
| Pathophysiology and Therapeutic Strategy for Diastolic Heart Failure. |
| Rick Nishimura |
| Mayo Clinic, Rochester, USA |
| |
Dr. Rick Nishimura, Mayo Clinic, USA, discussed the complex pathophysiology of diastolic heart failure (HF) using a simplified conceptual framework. The relationship between left ventricular and left atrial pressures as blood flows into the ventricle during diastole can be assessed using the mitral flow velocity curve. In the early stages of HF, although the systolic contraction remains normal, diastolic relaxation slows, producing symptoms upon exertion but not at rest. The mitral flow velocity curve reflects this slowed relaxation, as the ventricle is unable to fill properly during early diastole, with prolongation of flow deceleration and a compensatory increase in atrial contraction. As disease progresses, the curve shows a marked increase in initial velocity with a very fast flow, shortening the deceleration time.
|
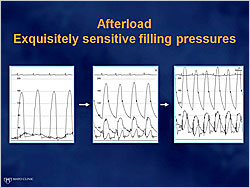
Figure 1. Afterload: Exquisitely sensitive filling pressures
【Click to enlarge】 |
|
|
Diastolic dysfunction progresses from normal function to relaxation abnormalities and terminates with compliance abnormalities. The Tajik Grading Scale can be used to grade the progression of diastolic dysfunction based on the mitral flow velocity curve. In a patient with a relaxation abnormality, a stress such as ischemia or hypertension results in severe dyspnea due to HF. If a patient with a near normal filling pressure at rest has a marked rise in blood pressure, the filling pressure increases, resulting in pulmonary edema even though a normal EF is maintained (Figure 1). This going back and forth between abnormal relaxation and high filling pressures is termed ventricular vascular stiffness and explains why some patients suddenly go into HF after doing well for years.
|
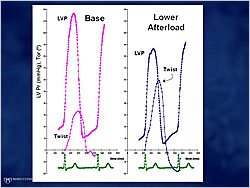
Figure 2. Effects of increased afterload on twist and untwist
【Click to enlarge】 |
|
|
High-resolution CT scan shows that the ventricle does not merely contract and relax but twists. The torsion is where the energy is stored; the untwist is where it is released. Echocardiography with speckle tracking and cardiac catheterization techniques show a twist during systole and an untwist during diastole that enhances ventricular relaxation, allowing the ventricle to fill. When an increased afterload blocks the ventricle’s ability to twist it cannot store energy and the untwist becomes abnormal (Figure 2). In patients with a severe abnormality of muscle stiffness causing class III/IV dyspnea, changes in load do not change filling pressures.
Conventional treatment of patients with diastolic dysfunction consists of reducing afterload and prolonging diastolic filling. Three new agents are under investigation for treating diastolic dysfunction. ALT-711 breaks extracellular matrix crosslinks, improving ventricle compliance. Ranolazine inhibits the Na+ channel, preventing Ca++ overload. The PDE5A inhibitor, sildenafil upregulates protein kinase G signaling and may enhance diastolic filling of the heart. |
| |
| Page Top |
|
| |
|
| Salt Loading Induces Left Ventricular Diastolic Dysfunction in a Metabolic Disorder Model. |
| Hiromitsu Matsui |
| University of Tokyo, Tokyo, Japan |
| |
Patients with metabolic syndrome (MS) have a highly increased risk for developing cardiovascular disease. Recent evidence has demonstrated that salt loading causes left ventricular (LV) diastolic dysfunction associated with increased oxidative stress and mineralocorticoid receptor (MR) activation. Dr. Hiromitsu Matsui, University of Tokyo, Tokyo, Japan, investigated the effects of high salt intake in rats with MS on cardiac diastolic function.
|
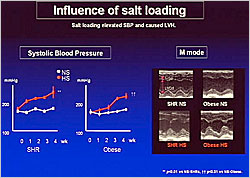
Figure 1. Influence of salt loading
【Click to enlarge】 |
|
|
Spontaneously hypertensive rats (SHR) and SHR/cp (obese) rats, a genetic model of MS, were fed a normal salt (0.5% NaCl) diet (NS) or a high salt (8% NaCl) diet (HS) for 4 weeks. The rats fed a HS diet developed elevated systolic blood pressure (SBP) and LV hypertrophy (LVH), both of which were significantly worse in the obese rats (p<0.01 for SBP and LVH) (Figure 1). Doppler echocardiography showed that the deceleration time of early mitral inflow was markedly elongated in the HS-obese rats versus the NS- and HS-SHRs (p<0.01) and the NS-obese rats (p<0.01). LV diastolic function was evaluated by the time constant in the LV pressure curve, showing that 4 weeks of a HS diet was enough to cause early LV diastolic dysfunction in the HS-obese rats (p<0.01 vs NS-SHRs and NS-obese rats). Salt loading also caused perivascular fibrosis of the coronary arteries in the HS-obese rats (p<0.05 vs HS-SHRs; p<0.01 vs NS-obese rats). The HS obese rats had significantly increased downstream gene expression of MR signaling.
The MR antagonist, eplerenone has been shown to significantly decrease proteinuria in HS-obese rats. Dr. Matsui found that eplerenone treatment shortened the deceleration time of early mitral inflow and the time constant in HS-obese rats versus untreated HS-obese mice (p<0.01), preventing early LV diastolic dysfunction. Eplerenone also prevented salt-induced perivascular fibrosis in the HS-obese rats. Unexpectedly, eplerenone normalized downstream gene expression of MR signals in HS-obese rats vs untreated HS-obese rats (p<0.05).
Reactive oxygen species (ROS) production was increased in HS-obese rats but normalized in eplerenone-treated HS-obese mice (p<0.01). When the antioxidant, tempol, was fed to the HS-obese mice, it shortened the deceleration time of early mitral inflow and the time constant and prevented perivascular fibrosis.
These results show that high salt intake is an aggravating factor for LV diastolic dysfunction, especially in the setting of MS. Salt induced activation of the aldosterone/MR system and downstream signals of MR and oxidative stress are involved in the pathogenesis of salt-induced early LV diastolic dysfunction in MS. MR antagonists or antioxidants are potential therapeutic strategies.
|
| |
| Page Top |
|
| |
|
| Cardiac Function and Hemodynamics in Diastolic Heart Failure using Left Ventricular Pressure-Volume Analysis. |
| Naoki Fujimoto |
| Mie University Graduate School of Medicine, Tsu, Japan |
| |
Dr. Naoki Fujimoto, Mie University Graduate School of Medicine, Tsu, Japan, presented the results of a study that compared cardiac function and hemodynamics during temporary inferior vena cava occlusion (VCO) and right atrial pacing in patients with diastolic heart failure (DHF) and those with systolic heart failure (SHF).
The study enrolled 37 consecutive patients admitted with DHF (N=20) or SHF (N=17). Hemodynamic measurements were made at the following time points: baseline; 15 minutes after baseline during VCO; 15 minutes later at steady state; 15 minutes after steady state during atrial pacing (20 bpm); and 10 minutes later during atrial pacing (40 bpm).
|
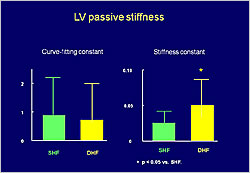
Figure 1. LV passive stiffness
【Click to enlarge】 |
|
|
Pressure volume (P-V) analysis showed that during VCO, end-diastolic volume (EDV) and end-systolic volume (ESV) were decreased in SHF and DHF patients. In both groups, diastolic P-V curves shifted downward with VCO. The average decrease in end-diastolic pressure (EDP) was smaller in DHF patients than in SHF patients (p<0.05). There was no difference in the curve-fitting constant between the two groups. The stiffness constant was greater in DHF patients than in SHF patients (p<0.05) (Figure 1).
|
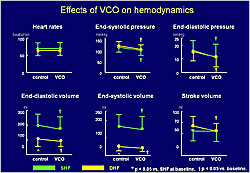
Figure 2. Effects of VCO on hemodynamics
【Click to enlarge】 |
|
|
VCO had no effect on heart rate in either group. VCO decreased end-systolic pressure (ESP), EDP, EDV, and ESV from baseline in both groups (p<0.05) (Figure 2). VCO had no effect on stroke volume in SHF patients but decreased stroke volume in DHF patients (p<0.05).
EDV decreased during atrial pacing at +20 bpm and +40 bpm in both SHF and DHF patients. Atrial pacing at +20 and +40 bpm had no effect on ESP in either group but decreased EDP in both groups (p<0.05). EDV and stroke volume decreased in both groups at +20 and +40 bpm (p<0.05). End-systolic elastance (Ees) was not affected by atrial pacing at +20 and +40 bpm in SHF patients but increased as heart rate increased in DHF patients (p<0.05). Effective arterial elastance (Ea) increased at +40 bpm in SHF patients and increased as heart rate increased in DHF patients. Atrial pacing impaired LV and arterial coupling in both groups (p<0.05) and had no significant effect on the time constant of LV relaxation in either group.
In summary, the LV was stiffer and external constraint smaller in DHF than in SHF. The force-frequency relationship was preserved in patients with DHF but LV-arterial coupling was impaired as the heart rate increased. These results suggest the cautious use of preload reduction and avoidance of tachycardia in the treatment of patients with DHF.
|
| |
| Page Top |
|
| |
|
| Current Status and Future Perspectives of Diastolic Heart Failure in Japan: Possible Importance of Metabolic Syndrome |
| Yoshihiro Fukumoto |
| Department of Cardiovascular Medicine, Tohoku University Graduate School of Medicine, Sendai, Japan |
| |
Dr. Yoshihiro Fukumoto, Tohoku University Graduate School of Medicine, discussed a study of CHF in patients with metabolic syndrome (MetS) and a potential new therapeutic target.
A nationwide study of CHF associated with MetS was conducted in Japan. MetS was defined as waist ≥85 cm in males and ≥90 cm in females, plus two or more of the following: Early MetS–blood pressure (BP) 130/80-140/90 mmHg, glucose 110-126 mg/dL, and HDL <40 or triglycerides (TG) >150; Advanced MetS–BP >140/90 mmHg, glucose >126 mg/dL, and HDL <40 or TG >150.
The investigators assessed 3,440 patients with stage C/D symptomatic HF. Of these, 2,164 (62%) did not have MetS, 1,156 (35%) had advanced MetS, and 94 (3%) had early MetS. Among the males, 47% had MetS (43% advanced, 4% early), while 20% of the females had MetS (19% advanced, 1% early).
|
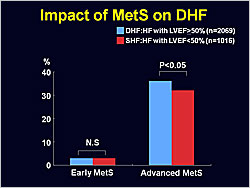
Figure 1. Impact of MetS on DHF.
【Click to enlarge】 |
|
|
|
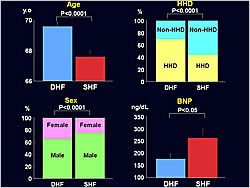
Figure 2. Features of DHF versus SHF patients.
【Click to enlarge】 |
|
|
The early MetS group had equal numbers of patients with DHF and SHF. More patients with advanced MetS had DHF than SHF (p<0.05) (Figure 1). The DHF group was characterized by older patients (p<0.0001), more females (p<0.0001), more hypertensive heart disease (HHD) (p<0.0001), and lower B-type natriuretic peptide (BNP) levels (p<0.05) than the SHF group (Figure 2).
A potential therapeutic target for DHF is Rho-kinase, which is involved in the pathogenesis of coronary artery spasm. Fasudil, a selective Rho-kinase inhibitor, inhibits acetylcholine-induced coronary artery spasm. Fukumoto’s laboratory investigated fasudil in male Dahl salt-sensitive hypertensive rats fed a high-salt diet from 7 to 17 weeks of age. The rats were randomized into three groups: 1) Untreated DHF, 2) DHF treated with low-dose fasudil, and 3) DHF treated with high-dose fasudil. Age-matched controls were maintained on a normal diet.
M-mode echocardiogram showed that LV wall thickness progressively increased in untreated DHF rats versus controls. LV wall thickening was inhibited in rats treated with high-dose fasudil (p<0.01 vs untreated DHF). LV end-diastolic diameter and fractional shortening were comparable among the four groups, indicating preserved LV systolic function. Doppler transmitral inflow velocity patterns showed that in the untreated DHF rats, the E/A ratio was reduced at 11 and 13 weeks (p<0.01 vs controls), then increased at 17 weeks, indicating a shift from delayed relaxation to a restrictive pattern, which was ameliorated in fasudil-treated DHF rats (p<0.05). Fasudil also ameliorated LV hypertrophy and lung edema (p<0.01).
Dr. Fukumoto concluded that treatment of metabolic syndrome and blockade of the Rho-kinase pathway might be novel therapeutic strategies for DHF.
|
| |
| Page Top |
|
| |
|
|