The use of drug eluting stents (DES) or coronary artery bypass graft (CABG) for patients with unprotected left main artery (ULMA) disease has been controversial in the United States. Dr. Richard A. Schatz, Scripps Clinic, La Jolla, California, USA, reviewed clinical trial data to clarify the relative roles of open heart surgery versus DES for ULMA disease.
|
Figure 1. Calcium Induced Calcium Release from SR
【Click to enlarge】 |
|
|
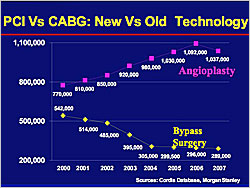
The number of percutaneous coronary intervention (PCI) procedures performed in the US has increased from 770,000 in 2000 to 1,037,000 in 2007, while bypass surgeries have dropped from 542,000 to 289,000 in the same period (Figure 1). Disadvantages of CABG include morbidity of the procedure; saphenous vein (SV) grafts are popular but are not as durable as left internal mammary artery (IMA) grafts; acceleration of underlying native coronary disease; and a 10-15% missed target rate during surgery.
The Society of Thoracic Surgeons (STS) 2006 database of 156,128 CABG patients shows that about 88% received left IMA grafts, while only 4.4% had bilateral IMA grafts and 7.7% had radial artery grafts. However, the most frequently implanted graft in the US is the SV graft. A 2005 study of patients receiving CABG showed that by 12 months 25% of SV grafts were occluded and 40% of patients had at least one occluded SV graft. About 8% of IMA grafts had failed after 12 months. A Cleveland Clinic study showed that SV graft patency was less than 40% after 5 years. Another study showed that SV graft failure was associated with profoundly increased death, myocardial infarction (MI), and revascularization. A 1981 Cleveland Clinic study reported that bypassed vessels had accelerated progression of underlying native disease versus vessels that were not grafted.
A meta-analysis showed no difference in mortality associated with PCI versus CABG. Another meta-analysis showed that there were higher rates of stroke with CABG (1.2%) versus PCI (0.6%) (p=0.002). In the PREVENT study of CABG plus edifoligide versus CABG plus placebo, both groups had similar rates of atrial fibrillation (25.1%, 26.7%), perioperative MI (9.6%, 9.9%), renal failure (3.2%, 3.3%), bleeding requiring reoperation (49%, 50%), pneumonia (33%, 37%), stroke (33%, 37%), ARDS (0.7%, 1.1%), mediastinitis (0.6%, 0.8%), and pulmonary embolism (0.8%, 0.3%). Lee et al reported that 53% of CABG patients had a morbid complication compared to only 1% of DES patients.
CABG surgery is indicated for patients with several restenoses or multiple failed interventions. Diabetics with diffuse disease, particularly if they have small vessels may need bypass surgery, although they are not good candidates for either PCI or CABG. Patients who have total occlusions with large and important territory at risk who are not amenable to PCI or who have failed PCI are good candidates for CABG. CABG also is appropriate in patients with excessive proximal tortuosity, particularly if the vessels are calcified and if they have good distal targets.
Chieffo et al reported good results after DES for ostial and shaft ULMA lesions in 147 patients, with 2.7% cardiac deaths, no MI, 0.7% target lesion revascularization (TLR), and 7.4% major adverse cardiac events (MACE). A Scripps Clinic study evaluated 9-month outcomes after ULMA PCI with DES in 106 patients. The results showed that the patients did poorly, with 3.8% cardiac deaths, 2.8% MI, 11.3% ischemic TLR, 32.1% any TLR, and 37.7% MACE. Most of the TLRs were a 2-stent strategy for a distal left main artery. An analysis of 17 observational studies showed that the greater the prevalence of distal left main disease, the greater the MACE. The presence of bifurcation disease was the most significant predictor of MACE and target vessel revascularization (TVR). Kim et al showed that simple ostial and shaft lesions have a very low restenosis rate (5.3%), while complex lesions that need a 2-stent strategy have a high restenosis rate (24.4%) (p<0.02).
IVUS is used liberally in ULMA interventions to define the lesion. A balloon pump is used if the patient has left ventricular (LV) dysfunction, severely elevated LV end diastolic pressure (LVEDP), critical right coronary artery (RCA) disease, a dominant circumflex branch, low blood pressure, or severely calcified distal left main coronary artery (LMCA).
For ULMA, a 1-stent technique should be used if possible, avoiding simultaneous kissing stent (SKS) unless speed and simplicity are critical. Post-dilation should be done with a non-compliant balloon at high pressure. IVUS should be done when finished and surveillance angiography performed at 3 to 9 months. Dr. Schatz found that about 40% of patients had critical in-stent restenosis with no symptoms.
The MAIN-COMPARE non-randomized study of patients with ULMA disease compared 396 patients matched for propensity scores who received DES or CABG. The investigators found no difference between the two groups in mortality or MACE at 3 years follow-up but the DES patients had a higher rate of TVR (p<0.001).
The Syntax trial randomized patients to CABG (N=897) or DES (TAXUS) (N=903). At the 12-month follow-up, TAXUS patients with left main disease had lower MACE rates than those who had CABG. Rates of death and MI in patients with multiple vessels were the same in the TAXUS and CABG groups but there was an almost 4-fold increase in stroke with CABG. The TAXUS patients had double the rate of repeat revascularizations, but according to Dr. Schatz these were relatively benign events.
Based on the available data, CABG is favored in patients with distal left main disease in the presence of: a clear need for a 2-stent technique; severely calcified vessels; concomitant chronic total occlusion of a dominant RCA; or concomitant severe 3 vessel disease. PCI is favored in the presence of: a favorable angle with little or no disease of the circumflex artery; non-dominant circumflex; or intangible factors not found in the EuroScore/Personnel score that might impact the duration or success of recovery, such as morbid obesity or mild dementia.
Dr. Schatz concluded that DES is indicated for unprotected left main lesions without surgical targets. Ad-hoc intervention is not unreasonable if the overall procedural risk is otherwise low. DES also is indicated for ostial and mid-shaft lesions, even in surgical candidates.
|