 |
|
|
 |
IS165
Evolving Clinical Applications of Tissue
Doppler Echocardiography |
|
John Gorcsan III, M.D.
University of Pittsburgh
Pittsburgh, PA, USA |
|
|
|
 |
|
|
 |
|
Circumferential shortening, longitudinal shortening,
and to a lesser extent rotational motion comprise the
principle vectors of left ventricular contraction. Longitudinal
shortening, expansion of the left ventricle (LV), and
the anatomic architecture of the superficial bulbo and
sinus spirals, the muscle fibers that wrap around the
mitral and tricuspid annulus and apex and contribute to
longitudinal shortening and lengthening of the LV, were
the focus of this lecture. Three clinical applications
of Tissue Doppler (TD) echocardiography (ECG) were discussed:
organ transplantation, differentiation of constrictive
pericarditis from restrictive cardiomyopathy, and assessment
of LV filling pressures.
|
PAGE
TOP
Physiology
of diastole and contraction |
|
 |
Figure
1. An example of color-coded mitral annular velocity
from an apical four-chamber view. (Gorcsan 2000)
Click
to enlarge |
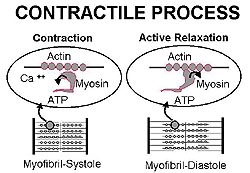 |
| Figure
2. A schematic of the contractile process in the
myocardium. (Gorcsan 2000) |
|
Considering longitudinal LV dynamics from the apical
view on routine ECG examination, movement towards
the transducer occurs during systole and movement
away from the transducer in diastole. This is opposite
of mitral inflow where movement is towards the transducer
in diastole. Figure 1 shows color-coded mitral annular
velocity from an apical four-chamber view.
The contractile
process is illustrated in Figure 2. Interaction
of the actin and myosin filaments consumes ATP in
systole causing a shortening of the myofibril and
in early diastole causing myofibril lengthening.
Energy is consumed throughout the contractile process,
so the early diastolic "E" wave is an active process that
contributes to LV suction and is affected by
myocardial diseases, such as ischemia, infiltrative
processes (cardiac amyloidosis), or transplant rejection.
TD and the longitudinal expansion velocities have
clinical relevance and application because of these
physiologic processes.
|
|
PAGE
TOP
|
Mitral annular motion and myocardial velocity gradient
on TD may be useful for detecting abnormalities
in ventricular function, and could potentially reduce
the number of biopsies (minimum 10/yr) that heart
transplant patients must undergo to predict rejection.
Preliminary data are promising and give hope that
the number of biopsies at least could be reduced;
more work is needed before biopsies can be eliminated.
In a patient
with moderate rejection, diminished systolic velocity
gradient and early diastolic gradient is seen. The
mitral annular velocity is affected in systole and
in particular in diastole, showing a markedly diminished
E wave amplitude. In another patient who underwent
sequential TD studies during moderate rejection
and then TD studies 6 months later, no rejection
was seen as evidenced by the increases in systolic
and diastolic velocity gradients and a more normal
pattern of mitral annular velocity.
In 84 patients who underwent TD studies at the
time of biopsy it was shown that mitral annular
velocity (combined systolic and diastolic peak velocities)
was the most predictive of transplant rejection.
The data had a 93% sensitivity, 71% specificity,
and a 98% negative predictive value.
|
|
PAGE
TOP
Differentiation
of constrictive pericarditis and restrictive cardiomyopathy |
|
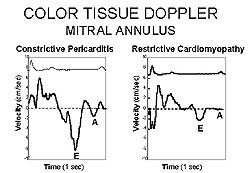 |
| Figure
3. The E wave is preserved on color TD in constrictive
pericarditis (left panel), whereas the E wave
velocity is diminished in restrictive cardiomyopathy
(right panel). (Gorcsan 2000) |
|
This is an exciting area now being applied in Gorscan's
lab, although these are rare diseases. Constrictive
pericarditis adversely affects ventricular filling.
Cardiac amyloidosis, an infiltrative disease, has
profound effects on diastolic function. Constrictive
pericarditis is treatable and can possibly be cured
with surgery, whereas cardiac amyloidosis has a
poor prognosis. In constrictive pericarditis there
is a peculiar filling abnormality with a rapid increase
in diastolic pressures followed by a plateau, as
shown by simultaneous hemodynamic tracings from
the right atrium, pulmonary artery, right ventricle,
and left ventricle. A similar pattern can be seen
with restrictive disease, making differentiation
difficult.
In constrictive pericarditis, the E wave is preserved
on color TD, whereas the E wave velocity is diminished
in restrictive cardiomyopathy, as shown in Figure
3. Pulse TD also shows the very diminished E wave
velocity in early diastole in restrictive cardiomyopathy.
Supportive data from the Cleveland Clinic shows
that mitral inflow and mitral annular velocity can
be used to differentiate restriction from constriction.
Gorscan recommends
these general guidelines to differentiate these
two diseases: In restrictive disease, the peak E
wave is usually less than 10 cm/sec with pulsed
TD and is usually less than 7 cm/sec with color
TD. Pulsed and color TD can be applied as complementary
techniques to mitral inflow and other data.
|
|
PAGE
TOP
Assessment
of LV filling pressures |
|
TD is used to assess LV filling pressures in routine
clinical practice at the University of Pittsburgh,
and is an exciting advance. Color-coded TD represents
mean velocities throughout the cardiac cycle, so
the peak systolic or diastolic velocity will be
much less compared with pulsed TD.
The ratio of mitral inflow velocity is compared
to the mitral annular velocity to predict LV filling
pressure. The inflow-to-annular (E/Ea) ratio has
been shown to correlate with mean pulmonary capillary
wedge pressure (PCWP) in a series of patients with
both normal and abnormal LV ejection fractions.
In patients with an E/Ea > 10, there is a 92%
sensitivity and an 80% specificity for having an
elevated filling pressure greater than 15 mm Hg.
In 180 patients with normal sinus rhythm or sinus
tachycardia TD was also shown to be useful (R=0.87),
representing another novel opportunity to assess
filling pressures.
|
|
PAGE
TOP
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2000
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|