 |
|
|
 |
IS146 Keynote Lecture
Transcatheter Assessment of Coronary Pathophysiology |
|
Morton J. Kern, M.D.
Department of Cardiology
Saint Louis University
Saint Louis, MO, USA |
|
|
|
 |
|
|
 |
|
The background, current status and future
use of physiologic methods to evaluate pathoanatomy were
reviewed. Employing these physiologic measurements has
uncovered a wealth of information in understanding the
coronary pathophysiology. A great deal of work remains
to understand this pathophysiology and improve therapeutic
modalities in coronary artery disease.
|
PAGE
TOP
|
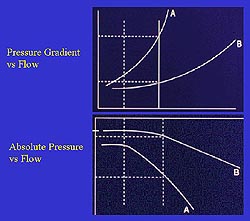 |
Figure
1. The basic concepts of lesion resistance, as
determined by the curvilinear relation between
flow increases and different degrees of pressure
loss, is the basis for measuring the physiology
of a coronary stenosis. (Kern 2000)
Click to
enlarge |
|
Pathophysiology is the combination
of disease effects influencing both the epicardial
conduit and the microvascular structure of the myocardium.
The conduits are connected through collateral channels,
which can be detected, quantitated and influenced
by pressure and flow variables. The microcirculation
is affected to varying degrees by different pathologic
conditions. Now the influence of a stenosis on coronary
flow as detected in the post-stenotic region can be
precisely quantitated using both pressure and flow
techniques.
Measuring the physiology of a coronary
stenosis is based on the basic concepts of lesion
resistance, as determined by the curvilinear relation
between flow increases and different degrees of
pressure loss (Fig. 1). The concept of fractional
flow reserve (FFR) advances the traditional concept
of determining the pressure gradient, the change
of pressure between proximal and distal portions
within the vessel, determining a greater degree
of pressure loss for any stenosis more severe than
another. In FFR the absolute distal perfusion pressure
is a measure of stenosis severity and the threshold
at which that stenosis can induce myocardial ischemia.
|
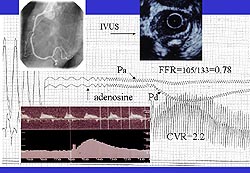 |
Figure
2. Angiogram and intravascular ultrasound (IVUS)
imaging provide precise anatomic detail, and measure
translesional pressure gradient and the absolute
pressure at maximal hyperemia. (FFR, fractional
flow reserve, CVR, coronary vasodilatory reserve;
Pa, aortic pressure; Pd, distal pressure). (Kern
2000)
Click to
enlarge |
|
Excellent tools for invasive and
intracoronary assessment of pathophysiology are now
available. The angiogram and intravascular ultrasound
(IVUS) imaging provide precise anatomic detail, and
can measure translesional pressure gradient and the
absolute pressure at maximal hyperemia (Fig. 2). FFR
is the difference between the aortic and distal pressure
at high hyperemia. The FFR has a well-defined threshold
below which myocardial ischemia in stable patients
is associated.
Coronary flow velocity is measurable
and can provide a graphic demonstration of the changes
in coronary flow over time and in response to different
stimuli (drug, exercise, intrinsic stimuli that
alter the coronary circulation). The influence of
different interventions over time on flow patterns
can be observed by using the measurement of flow
trending. Combining the two measures of change in
pressure and change in flow, results in an absolute
precise determination of the entire coronary circulation,
both the response at the epicardial level and at
the microvascular level.
|
|
PAGE
TOP
Using physiology
to understand abnormal coronary pathophysiology |
|
| Different measurements of
coronary stenoses, single lesions, addressing diffuse
coronary artery disease (CAD) with FFR and coronary
flow reserve (CFR), and myocardial infarction (MI) and
flow were reviewed. Collateral circulation, microcirculatory
status, endothelial dysfunction, and vasospasm can also
be assessed, but were not discussed in this lecture.
|
|
PAGE
TOP
Coronary
pressure measurements |
|
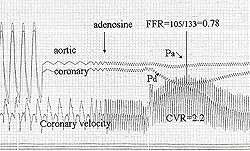 |
Figure
3. Increasing coronary flow through the coronary
stenosis increases the distal pressure in proportion
to the resistance in an exponential fashion. (FFR,
fractional flow reserve, CVR, coronary vasodilatory
reserve; Pa, aortic pressure; Pd, distal pressure).
(Kern 2000)
Click to
enlarge |
|
Pressure guide wires have been developed
to measure distal pressure and proximal aortic pressure.
FFR has become critically important to the complete
understanding of when a stenosis is significant enough
to cause myocardial ischemia and warrant coronary
intervention. As coronary flow increases through a
coronary stenosis, the distal pressure loss increases
in proportion to the resistance in an exponential
fashion (Fig. 3). That pressure loss can be caused
by friction, turbulence, separation, or the energy
of flow being taken out as heat, thus the pressure
loss is distal to that stenosis.
FFR and myocardial ischemia
FFR is the ratio of absolute distal
pressure to proximal pressure at maximal hyperemia.
FFR is defined as a percentage of the normal flow
going through an artery in the absence of the stenosis.
(FFR = the ratio of flow through the stenotic vessel
(QS) over the ratio of flow in the theoretic normal
value (QN) (FFR= QSmax/ QN max.) When resistance
is minimal, the simple equation of distal pressure
over aortic pressure measured at maximal hyperemia
(Pa/Pd) can be used. When this percentage is less
than 75%, it has a very strong association with
inducible myocardial ischemia in stable patients.
FFR is based on a fixed resistance
and is specific for the stenosis resistance, thus
it is independent of variables that influence coronary
flow reserve, such as heart rate, blood pressure,
and contractility that can influence basal and hyperemic
flow. Work by Pijls has shown that the reproducibility
of CFR under different hemodynamic conditions is
not as strong as is the reproducibility with FFR.
CFR measures both the stenosis and
the effect of the myocardial bed, and is thus a
composite measure. Measuring relative coronary flow
reserve (rCFR), the ratio of CFR in a reference
vessel to that in a target vessel, eliminates the
influence of the myocardial bed and increases specificity.
FFR or concepts using pressure-derived FFR can begin
to inform about the influence of collateral circulation
on myocardial ischemia.
The relation between absolute CFR
and FFR is not very strong, as CFR measures both
the microvascular bed and the conduit. There is
a stronger relation between the rCFR and FFR, by
eliminating the microvascular bed. In some conditions,
rCFR is thought to be a more lesion-specific measure.
More work in this area is forthcoming to determine
the relation of rCFR to myocardial ischemic stress
testing.
Comparison of FFR and CFR
Hemodynamic and microvascular independence
are both related to rCFR and FFR. The normal value
for FFR is 1.0, and for rCFR it is a range greater
than 0.8. A CFR value greater than 2 is associated
with normal ischemic stress testing. FFR and CFR,
but not rCFR, can be employed in multiple vessel
disease. The collateral circulation can be assessed
using CFR measured during balloon angioplasty and
FFR measured with a pressure wire during balloon
occlusion.
The relation between CFR in the post-stenotic
region and positive stress testing has been examined.
Values less that 2 are associated with positive
ischemic stress testing, ranging from adenosine,
sestamibi, exercise thallium, dipyridamole echo,
and exercise ECG. This is based on a number of studies
during the past five years that have relatively
high sensitivity (ranging from 82-100%), specificity
(71-100%) and predictive accuracy (86-96%).
FFR values less than 0.75 are associated
with myocardial ischemia, based on data in patients
with stable angina. Such values for AMI or UA have
not been developed and are the subject of future
testing.
|
|
PAGE
TOP
|
|
|
Angiograms are not always reliable
in assessing diffuse CAD. For example, when CFR
is measured in the right coronary artery (RCA) a
value of 2.8 can be generated, whereas a value of
1.6 can be generated through the diseased left coronary
artery (LCA). In this case, it is likely that benefit
will be obtained by dilating the LCA region, rather
than by dilating the RCA region.
Deferring treatment of intermediate
stenoses with normal physiology results in good
clinical outcomes. The safety of the technique and
the long-term events in these patients are low,
equivalent to those patients with CAD that is inactive
and treated. Multiple studies using FFR or CFR indicate
a 10% or less event rate for progression of disease
in intermediate lesions having undergone physiologic
evaluation with sensor guidewires.
|
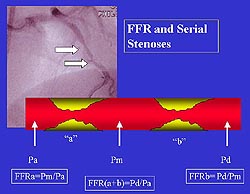 |
Figure
4. Calculation of the fractional flow reserve
in serial stenoses. (FFR, fractional flow reserve;
Pa, aortic pressure, Pm, middle pressure; Pd,
distal pressure) (Kern 2000)
Click to
enlarge |
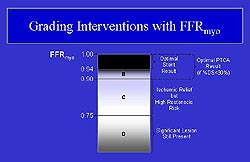 |
Figure
5. Fractional flow reserve grading criteria for
myocardial interventions. (Kern 2000)
Click to
enlarge |
|
Serial stenoses
Determining whether FFR can be useful
in identifying which stenosis of serial stenoses
may be important to dilate has been an area of recent
investigation. The concept and the mathematics used
to derive the equations can be somewhat complex.
To consider the FFR between lesions requires knowing
the relation between the pressure between lesion
A and lesion B (Fig. 4). The FFR for lesion A is
derived as a distal pressure of the middle section
versus the aortic pressure. Lesion B is the distal
pressure divided by the middle pressure. The classic
FFR is the sum of the two stenoses. Changing the
resistance across one lesion will change the flow,
and thus will impact the re-calculation of the second
lesion. This use is forthcoming.
Use of physiology during interventions
A case study illustrated employing
physiology during interventions. A severe stenosis
in a circumflex artery is associated with an abnormal
and very low FFR of 0.38, a CFR of 1.1, and rCFR
of 0.5 when the unaffected left anterior descending
(LAD) has an FFR of 2.0. Angioplasty alters the
pathophysiology. Although the anatomic result may
be acceptable, the physiologic result, at least
based on a CFR of 1.5, is unacceptable. In most
cases this is due to material remaining in the artery
that can be pushed aside with stenting, and in many
cases this normalizes the FFR to 2.0 and creates
an rCFR of 1.0. This is a classic example. CFR may
not normalize in about 20% of patients and microcirculatory
abnormalities may persist, despite having a normal
FFR or rCFR. The FFR grading criteria for interventions
is shown in Figure 5.
Physiologically-guided PTCA and
stent
Provisional stenting is no longer
practiced. However, three studies (DEBATE-II, DESTINE-CFR,
FROST) indicate that about 50% of the time stent-like
results can be achieved with balloon-angioplasty
guided by a physiologic endpoint. A study by Bech
et al found about a 15% 2-year target lesion revascularization
rate when a good anatomic angioplastic endpoint
was achieved with an FFR greater than 0.90.
|
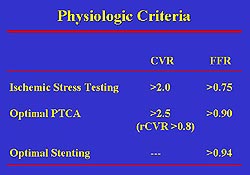 |
| Figure
6. Physiologic criteria for coronary flow reserve
and fractional flow reserve. (Kern 2000) |
|
Physiologic criteria in ischemic
stress testing
The criteria for CFR and FFR in ischemic
stress testing were summarized (Fig. 6). For each
test, there is small gray zone, larger for CFR than
for FFR. Thus, not every 0.75 stenosis requires
dilation and clinical judgment must be employed.
The estimated rCFR threshold value is greater than
0.8. But, no definitive studies have been published
to support this value, and there is a little broader
gray zone. Angioplasty endpoints in the DEBATE trial
show that CFR values greater than 2.5 with good
anatomy were associated with low event rates. FFR
values greater than 0.90 were also associated with
very satisfactory if not superior endpoints, based
on data from Pijls. An FFR greater than 0.94 indicates
the stent is fully deployed, when validated by IVUS.
A multicenter trial is underway in the United States
to evaluate whether FFR can be used to define the
endpoint in stenting.
Assessment of diffuse CAD after
stenting
What is the best way to assess if
flow has been well restored in the setting of a
severe LAD lesion with a well-stented segment, but
a diffusely diseased distal vessel? When measuring
FFR, initially there is a loss of distal pressure
across the stenosis but no further pressure loss
with adenosine. Despite achieving good anatomic
results with stenting, CFR was impaired. The use
of pressure and flow measures can help to determine
whether the angioplasty in the proximal LAD is not
as good as it looks (hidden material or an unappreciated
segment), or if there is microvascular impairment,
or abnormal conductance of the LAD segment, or a
combination of these factors.
In this case, the FFR was normal when
measured distal to the stent and in the proximal
portion of the artery. The stent was perfectly expanded,
placed well, and conductance up to that point in
the arterial segment was normal. Measuring distally
to the segment showed there was a mass of material
in the vessel (the diffuse CAD) that was producing
a gradual but continual pressure loss. When the
FFR was measured in the distal region it was very
abnormal. A hyperemic pull-back performed from the
distal to the proximal vessel during infusion of
intravenous adenosine showed there was a gradual,
subtle decrement in the pressure gradient and improvement
in pressure as it went up to the stent, indicating
a long, diffuse segment of disease. Regardless of
how well the epicardial conduit is treated, perfusion
down the distal vessel is not possible due to the
plaque accumulation. Treating focal stenoses along
the vessel will not result in improvement.
|
|
PAGE
TOP
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2000
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|