| |
 |
|
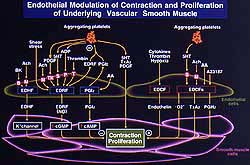
Figure
1. Endothelial modulation of contraction and
proliferation of underlying vascular smooth
muscle. (Shimokawa 2000)
Click
to enlarge
|
 |
|
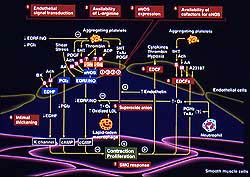
Figure
2. Schematic of mechanisms of endothelial dysfunction
in atherosclerosis. (Shimokawa 2000)
Click
to enlarge
|
|
Endothelial cells possess vasodilator function,
as well as anti-thrombotic and anti-inflammatory
functions. This summary lecture reviewed the importance
of endothelial dysfunction, methods to assess endothelial
function in humans and their limitations, and therapeutic
implications.
Endothelial cells synthesize at least three different
vasodilator factors: nitric oxide, prostacyclin,
and an unidentified endothelium-derived hyperpolarizing
factor (EDHF), as shown in Figure 1. Under several
pathological conditions, endothelial cells also
synthesize several vasoconstricting factors (EDCF),
including endothelin, superoxide and vasoconstrictor
prostaglandin (Fig. 1).
Animal and human studies have demonstrated several
mechanisms are involved in endothelial dysfunction
(ED) in atherosclerosis (Fig. 2), including:
- reduced or impaired endothelial signal transduction
- reduced availability of L-arginine
- reduced eNOS expression
- reduced co-factor for eNOS
- NO inactivation increased by superoxide anion
derived from macrophages other inflammatory
cells, endothelial cells
- concomitant release of EDCF
- intimal thickening (possible diffusion barrier)
- smooth muscle vascular response
|
|
PAGE
TOP
NO-mediated
regulation of coronary blood flow |
|
Under various conditions, including the presence
of coronary risk factors, coronary artery disease
(CAD), heart failure, or left ventricular (LV) hypertrophy,
NO-mediated responses are impaired under basal conditions
or in response to acetylcholine or other stimuli,
such as metabolic or exercise stimuli.
ED appears to have prognostic value for patients
with ischemic heart disease (IHD). A group from
Germany reported that with good coronary vasodilator
responses to increased flow, prognosis is very good.
But, with impaired flow-mediated vasodilation the
prognosis worsens. Flow-mediated dilatation greater
than 15% is associated with a 90% survival rate
at 10 years, 11-19% flow-mediated dilatation with
a 90% survival, and less than 11% flow-mediated
dilatation about a 60% survival. The group with
less than 11% flow-mediated dilatation also had
impaired endothelium-independent relaxation to nitrovasodilators.
Shimokawa thinks it remains unproven whether ED
truly has prognostic value, for example in patients
with IHD or heart failure.
|
|
PAGE
TOP
Assessment
of endothelial function in humans |
|
|
|
In vitro analysis of isolated human blood vessels
Endothelial function
can be assessed in freshly isolated blood vessels
from humans. Bradykinin caused greater relaxation
in the large arteries and resistant small mesenteric
arteries, compared to acetylcholine, in one study
of endothelium-dependent relaxation (EDR). The bradykinin-induced
EDR in the large arteries was due to the combined
effect of NO and EDHF, as shown by one-half being
sensitive to L-arginine and one half to KCl in the
presence of indomethacin and L-arginine. However,
in the microvessels bradykinin-induced EDR was insensitive
to L-arginine and highly sensitive to KCl in the
presence of indomethacin and L-arginine, indicating
the relaxation was largely mediated by EDHF but
not NO.
|
 |
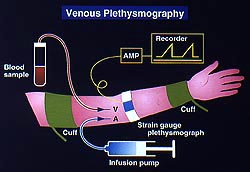
Figure
3. Flow-mediated endothelium-dependent relaxation
can be assessed non-invasively in vivo by continuously
measuring the brachial artery diameter change
in response to occlusion and reflow. (Shimokawa
2000)
Click
to enlarge |
 |
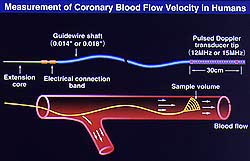
Figure
4: In vivo invasive assessment of endothelial
function with venous plethysmography can accurately
measure forearm blood flow response and allows
for venous blood collection. (Shimokawa 2000)
Click
to enlarge |
 |
|
Figure
5. The endothelial function of both the large
epicardial coronary artery and the microvasculature
can be assessed by combining quantitative coronary
angiography and Doppler wire assessment, which
can continuously monitor diameter changes in
large coronary arteries and changes in coronary
blood flow. (Shimokawa 2000)
Click
to enlarge
|
|
In vivo non-invasive assessment
Ultrasound is
used to measure flow-mediated dilatation for non-invasive
in vivo analysis, and is particularly useful in
the clinical setting. By continuously measuring
the brachial artery diameter change in response
to occlusion and reflow, as demonstrated in Figure
3, the flow-mediated EDR can be assessed. The disadvantage
of this technique is that the relation between brachial
artery response and coronary artery response is
unclear. There is ongoing controversy about whether
this brachial artery response truly represents the
coronary artery response, and more studies are needed.
In vivo invasive assessment
Invasive in vivo
analyses use 1) venous plethysmography of forearm
circulation (Fig. 4) and 2) quantitative angiography
(QCA) and Doppler flow wire assessment of coronary
circulation (Fig. 5). More accurate evaluation of
endothelial function is obtained with these techniques.
Combining QCA and Doppler flow wire allows continuous
monitoring of the changes in diameter in large coronary
arteries and in coronary blood flow, thus assesses
both large epicardial coronary artery endothelial
function and microvascular endothelial function.
Biochemical markers
Several biochemical markers could be used as an
indicator of endothelial function: NOx plasma level,
prostacyclin, thrombomodulin von Willebrand factor,
and tissue factor pathway inhibitor, among others.
A combination of these markers may help to assess
endothelial function systemically.
|
|
PAGE
TOP
Limitations
of clinical assessment techniques |
|
The relative contribution of NO, EDHF and prostacyclin
must be considered.
A study by Shimokawa in porcine large epicardial
arteries and in coronary microvessels showed that
1) prostacyclin contribution was minimal in large
and small arteries, 2) NO contribution was greater
in large coronary arteries, and 3) EDHF contribution
was greater in smaller vessels. Further, in pig,
rabbit, mice, rat and human vessels he demonstrated
1) NO contribution was greater in large blood vessels,
2) EDHF was greater in microvessels. This observation
must be considered when assessing endothelial function,
even in humans.
To assess the effect of shear stress on endothelial
function, an in vitro system to continuously monitor
the change in diameter in isolated blood vessels
and change perfusion pressure and blood flow was
developed by Shimokawa. NO and EDHF contributed
to shear stress-induced EDR in the large rat arteries,
but EDHF contribution was greater than NO in the
rat arteriole.
Contribution of vascular smooth muscle responses
Vasospasm and ED must be differentiated when assessing
endothelial function in humans. In a coronary angiography
study, no stenotic lesion was seen under basal conditions.
A marked hyperconstriction (vasospastic response)
was observed after intracoronary administration
of acetylcholine. This response disappears after
intracoronary nitroglycerine administration. This
phenomenon might be considered ED.
However, in an animal model of coronary hyperconstriction
(developed by chronic treatment of the porcine coronary
artery with the inflammatory cytokine interleukin-1beta),
marked hyperconstriction occurred after serotonin
stimulation.
Surprisingly, bradykinin- or calcium ionophore-induced
EDR was fairly preserved at the site of vasospasm.
Responses were fairly preserved to the vasospastic
agonist serotonin.
Direct evaluation of EDR in response to serotonin
was possible because ketanserin, a 5HT2A serotonergic
receptor blocker, was used to directly inhibit vascular
smooth muscle contraction. This contraction was
significantly augmented at the spastic segment in
blood vessels without endothelial cells in response
to serotonin, compared to control segments. The
hypercontraction responses of the coronary artery
were achieved mainly by a hypercontraction of vascular
smooth muscle, rather than by ED, at least in their
porcine model.
Variable responses to different agonists
Endothelial dysfunction
does not occur uniformly to all agonists, but rather
in a step-wise manner. At least two signal transduction
pathways are involved with the production of NO
from endothelial cells. One is mediated by the Gq-protein
and the other by the Gi-protein, as demonstrated
by Shimokawa. Serotonin, norephinephrine, and endothelin
are among the agonists that use the Gi-protein mediated
pathway. ED occurs in a step-wise manner, rather
than uniformly, during the process of atherosclerosis,
also demonstrated by Shimokawa. In the early stage
of atherosclerosis, the Gi-protein mediated pathway
becomes impaired, and in the middle of atherosclerosis
pathways mediated by other G proteins are impaired.
However, until the advanced stage of atherosclerosis
eNOS function is preserved or is increased in atherosclerotic
endothelial cells.
Studies of the effect of hypercholesterolemia on
vasodilator function in animals and humans show
that EDR to acetylcholine or serotonin is easily
impaired. But, in response to bradykinin or calcium
ionophore it is fairly preserved. Therefore, if
possible, at least two agonists must be used to
completely test endothelial function. Aging impairs
endothelial vasodilator effects. Studies show that
aging easily impairs EDR to acetylcholine in humans,
but that bradykinin-induced EDR is not significantly
influenced by age.
|
|
PAGE
TOP
|
Correction of underlying risk factors, such as
hyperlipidemia, hypertension, diabetes, and smoking,
has been demonstrated to improve EDR in patients
with IHD or heart failure. The use of fish oil,
estrogen replacement therapy, ACE inhibitors, anti-oxidant
agents, and probably L-arginine are also beneficial.
Fish oil studies
EDR was normalized
in patients with CAD treated for 6 weeks with eicos-spentacnole
acid (EPA), a major component of fish oil. Venous
plethysmography studies showed that forearm vasodilation
responses to acetylcholine and substance P were
impaired before EPA treatment, but were normalized
after treatment. Interestingly, the acute administration
of L-NMMAæ abolished the improved EDR in response
to acetylcholine, but did not significantly reduce
the relaxation in response to substance P, indicating
that EDR mediated by NO and EDHF is impaired in
patients with CAD. Long-term treatment with EPA
may improve both NO-mediated and EDHF-mediated relaxation.
EPA treatment can improve endothelial vasodilator
functions in human coronary circulation of patients
with IHD. Shimokawa demonstrated that long-term
treatment with fish oil markedly augmented the EDR
of the coronary artery in response to aggregating
platelets in both the porcine model and humans.
Before EPA treatment, the patients showed no increase
in coronary flow in response to acetylcholine, indicating
very impaired coronary vasodilator responses. However,
after 6-8 weeks of EPA treatment, the blood flow
response was normalized.
Estrogen study
Estrogen treatment
improved NO-mediated and probably EDHF-mediated
relaxation in post-menopausal women. Estrogen normalized
forearm blood pressure responses to acetylcholine
and substance P in post-menopausal women. Acute
administration of L-NMMA in the forearm circulation
inhibited the acetylcholine-induced increase in
flow, but not the substance P-induced increase.
|
|
PAGE
TOP
|
The relative contribution of prostacyclin, NO and
EDHF to EDR, based on Shimokawa§fs view is:
- NO and EDHF mainly contribute to EDR under normal
conditions, although there are many redundancies
between NO and EDHF.
- NO-mediated relaxation is impaired first during
atherosclerosis with several coronary risk factors.
- EDHF-responses seem to be upregulated for a
while to maintain EDR.
- EDHF-responses become impaired as atherosclerosis
progresses.
- NO- and EDHF-mediated EDR is reduced at the
most advanced stage of atherosclerosis.
- Prostacyclin seems to play a compensatory role.
- NO-mediated and then EDHF-mediated responses
are recovered with risk factor correction or drug
treatment.
To examine the
prognostic value of ED, the ENCORE trial is being
conducted. ENCORE I is addressing the relatively
short-term effects (6 months) of treatment with
nifedipine, cerivastatin, or both, to determine
their ability to improve endothelial vasodilator
function, evaluated by QCA and Doppler flow wire.
ENCORE II is addressing the long-term (2 years)
effect of nifedipine and simvastatin using QCA and
IVUS. This trial will determine the clinical importance
of ED and the importance of its correction on the
structural changes of the coronary artery and the
prognosis in patients with IHD. Future trials will
determine the importance of ED in humans.
|
|
PAGE
TOP
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2000
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|