Oxidative Stress Predicts Cardiovascular Events |
|
Oxidative stress in polymorphonuclear leukocytes
(PMNs) and mononuclear cells (MNCs) may be independent
predictors of the risk for cardiovascular events,
according to a large study conducted by Osaka City
University investigators.
Kenichi Yasunari and colleagues conducted a prospective
study of 529 subjects followed for a mean of 1 year
to study the association between PMN and MNC oxidative
stress and cardiovascular events. Cardiovascular events
were defined as heart failure, need for coronary revascularization,
and stroke. Intracellular oxidative stress of PMNs
and MNCs was measured by gated flow cytometry using
carboxyfluorescin diacetate bis-acetoxymethyl ester.
In vitro studies had previously shown that oxidative
stress in smooth muscle cells can be increased by
chronic high glucose administration, oxidized LDL
cholesterol, and high blood pressure
Traditional risk factors were also evaluated, including
age, sex, body mass index, lipid levels, hemoglobin
A1c, and mean blood pressure, as well as the nontraditional
risk factors of insulin action, homeostatis model
assessment (HOMA-IR), and C-reactive protein. The
study population was divided into four groups: normotensive
subjects with no diabetes; hypertensive subjects with
no diabetes; normotensive subjects with diabetes;
and hypertensive subjects with diabetes.
|
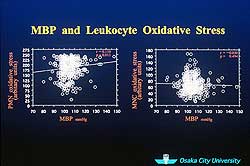 |
| Figure
1. PMN but not MNC oxidative stress increased
as mean blood pressure increased. |
| Click
to enlarge |
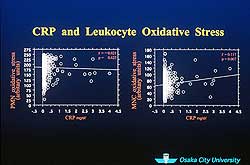 |
| Figure
2. A significant relationship between increasing
levels of C-reactive protein and MNC oxidative
stress was found, but not between increasing C-reactive
protein and PMN oxidative stress. |
| Click
to enlarge |
|
Multiple regression analysis showed a significant
relationship between mean blood pressure and PMN oxidative
stress (r = 0.115; p = 0.012); as mean blood pressure
increased, PMN but not MNC oxidative stress increased
(Figure 1). There was also a significant relationship
between increasing C-reactive protein and increases
in MNC but not PMN oxidative stress (r = 0.121; p
= 0.625) (Figure 2). Also, as hemoglobin A1c increased,
PMN and MNC oxidative stress increased. With regard
to the subsets of subjects, the most significant increase
in PMN and MNC oxidative stress was observed in the
hypertensive/diabetes group.
In sum, an increase in PMN oxidative stress was significantly
related to higher levels of blood pressure and hemoglobin
A1c. An increase in MNC oxidative stress was significantly
related only to C-reactive protein, suggesting a link
to vascular inflammation.
During 1 year of follow-up, there were 56 cardiovascular
events among the 529 subjects: 39 strokes and 17 cases
of heart diseases, including 11 cases of heart failure
and 6 nonfatal myocardial infarctions. A case-control
study showed that both PMN and MNC oxidative stress
was increased in cases versus controls, but the other
traditional and nontraditional risk factors were not
different.
According to a Cox proportional analysis, both PMN
and MNC oxidative stress were significantly predictive
of the risk of a cardiovascular event, even after
an adjustment for other risk factors. In fact, among
all 12 risk factors, the only significant predictive
factors were PMN oxidative stress, for which the relative
risk was 1.48, and MNC oxidative stress, with a relative
risk of 1.28. The results suggest that hypertension
leads to the activation of PMNs and that C-reactive
protein is related to MNC oxidative stress. The measurement
of PMN and MNC oxidative stress may help identify
risk of future cardiovascular events, Dr. Yasunari
predicted.
|
PAGE
TOP
|
A Novel Marker of Stent Restenosis |
|
Asymmetrical dimethyl-arginine (ADMA), an endogenous
inhibitor of nitric oxide synthase, is a novel marker
of vascular endothelial dysfunction and atherosclerosis.
Plasma levels of ADMA may also predict which patients
will experience restenosis after stent implantation,
according to a multicenter study presented at the
meeting by Masashi Fujita of Kansai Rosai Hospital,
Amagasaki.
Neointimal hyperplasia after stent implantation is
partially due to endothelial activation, and reduction
of nitric oxide release causes endothelial dysfunction.
To check the relation between the plasma level of
ADMA, nitric oxide and stent restenosis, the investigators
measured the plasma level of ADMA and the end-products
of nitric oxide in 37 patients (mean age 65) with
coronary artery disease before stent implantation
and after 6 months.
The plasma level of ADMA was measured by high-performance
liquid chromatography and nitric oxide was measured
by the Griess method. Intravascular ultrasound (IVUS)
was also performed on all lesions before and 6 months
after stent implantation. Stent volume and intimal
hyperplasia volume were calculated by 3-dimensional
IVUS analysis with 0.5-mm intervals throughout the
stented segment, and the percent volume stenosis was
calculated. Pre-stent reference diameter was 2.79
mm, minimal lumen diameter was 1.15 mm, and diameter
of stenosis was 60%. Post-procedure, these numbers
were 3.29 mm, 2.93 mm, and 11.78%, respectively.
|
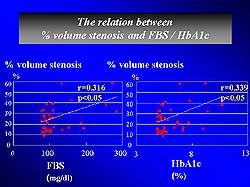 |
| Figure
3. A significant correlation was found between
percent volume restenosis and fasting blood sugar
and hemoglobin A1c. |
| Click
to enlarge |
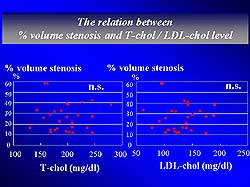 |
| Figure
4. Percent volume restenosis and LDL or total
cholesterol showed no association. |
| Click
to enlarge |
|
Indeed, baseline ADMA levels seemed to predict the
risk for stent restenosis. The plasma level of ADMA
before stent implantation was much higher in patients
with progressive neointimal hyperplasia than non-progressive
neointimal hyperplasia. Since patients with type 2
diabetes have an increased risk for restenosis, ADMA
levels were examined separately in these patients
and found to be significantly higher in diabetics
than in patients without type 2 diabetes.
Percent volume restenosis was also significantly
correlated with the baseline plasma ADMA level. The
higher the ADMA level, the more progressive the neointimal
hyperplasia. Percent volume restenosis was also correlated
significantly with fasting blood sugar and hemoglobin
A1c (Figure 3). No association was found between percent
volume stenosis and LDL or total cholesterol levels
(Figure 4). The investigators concluded that the plasma
level of ADMA is important in the pathophysiology
of neointimal hyperplasia and may be a predictor of
coronary stent restenosis.
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2002
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|