 |
|
|
 |
| ACS: Prevention to Treatment |
|
|
|
 |
|
Pathogenetic
Perceptions of Acute Coronary Syndrome: Insights into
Plaque Rupture, Plaque Erosion and Coronary Thrombosis
in Japanese
Hiroyuki Hao
National Cardiovascular Center,
Osaka, Japan
|
|
Rupture of unstable plaque is a major cause of acute
coronary syndromes (ACS). However, in 2000, Virmani
and colleagues proposed a modified classification
of coronary atherosclerotic lesions, based on their
observations of more than 200 cases of sudden cardiac
death (SCD). Based on their observation of the lack
of a relationship between SCD and the classic AHA
classification, their modified classification focuses
on the intermediate or advanced lesion, and indicates
seven different categories of lesions. Lesions with
thrombus, which causes ACS, including SCD, exhibited
3 distinct processes: rupture, erosion, calcified
node. Regarding erosion, they noted a cycle that can
be continuous. Intimal thickening progressed to pathologic
intimal thickening and to erosion, which can lead
to thrombosis and SCD or to thrombosis, and then healing
and formation of a fibrocalcific plaque, which can
be followed by a new erosion; this cycle can then
continue.
Rupture of the fibrous cap is often seen in the
shoulder of the lesion, followed by focal foam cell
infiltration. Erosion is identified when serial sectioning
of thrombosed coronary artery fails to reveal plaque
rupture. Surprisingly, the eroded lesion shows minimal
inflammation. In the US, about 40% of SCD is associated
with lesion erosion. It is more common in men and
women below 50 years of age and is associated with
smoking, especially in women.
Virmani and colleagues examined the accumulation
of extracellular matrix at the erosion site of the
culprit lesion to understand the mechanisms of erosion.
Staining showed strong presence of versican and bHABR,
but biglycan and decorin were weak. The fibrous cap
of stable plaque showed strong bigylcan and weak bHABR
staining.
Further investigation by Gabbiani, Bochaton-Piallat
and Virmani focused on cell density and smooth muscle
(SM) cell differentiation in the erosion. They examined
the expression of alpha-SM actin, smooth muscle myosin
heavy chain (SMMHC), and smoothelin, which are all
well accepted SM cell differentiation markers. In
the intima, a high density of alpha-SM actin positive
cells was found, weak expression of SMMHC, and no
staining of smoothelin by histochemistry. In the intima,
the degree of differentiation of SM cells was significantly
lower than in stable plaque—suggesting that plaque
erosion may have a close connection with the phenotype
of the intimal SM cells, as myofibroblastic phenotype.
|
|
Erosion in lesions in Japanese AMI patients
|
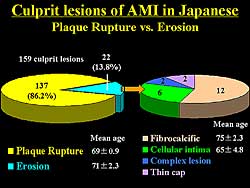 |
| Figure
1. The disposition of culprit lesions of acute
myocardial infarction in Japanese patients |
| Click
to enlarge |
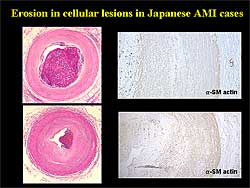 |
| Figure
2. Erosion of cellular intima in Japanese cases.
Diffuse intimal thickening with occlusive thrombus
formation is seen in the right coronary artery,
with no lipid in the intima. Alpha-SM actin staining
is minimal, indicating less cell differentiation
compared to normal media or advanced lesion intima.
|
| Click
to enlarge |
|
In 159 carotid lesions in Japanese patients with
an AMI analyzed by Hao and colleagues, plaque rupture
was the cause of death in 86%, and erosion in
14% of patients (Figure 1). Notably, the mean age
of the patients with erosion as the cause of death
was 71 years, significantly older than the US patients
with SCD due to erosion.
Based on histological features, they classified
the erosions into 4 different categories: fibrocalcific
lesions and fresh thrombus in 12 cases, eroded cellular
intima in 6, complex lesion in 2, and thin fibrous
cap in 2 cases.
In the fibrocalcific lesions, extracellular matrix,
which was very often calcification, was accumulated.
In eroded fibrous atheroma, mature extracellular matrix
was present, and alpha-SM actin in media and especially
intima thickening on immunohistochemistry.
The broad density of alpha-SM actin positive cells
in the intima was quite different in the Japanese
AMI patients compared to SCD in the US.
In the 6 Japanese cases of eroded cellular intima,
there was diffuse intimal thickening with occlusive
thrombus formation in the right coronary artery; the
intima contained no lipid (Figure
2). The medial SM cells had a minimal reaction
with alpha-SM actin, indicating these cells are less
differentiated compared to the normal media or media
in advanced lesions. In the cellular intima, alpha-SM
actin positive cells were seen, which is similar to
erosion in SCD in the US.
|
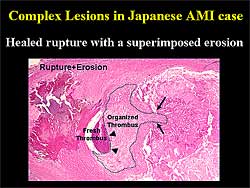 |
| Figure
3. The multiple complications in complex lesion
include plaque rupture and erosion. A healed rupture
can be followed by fresh thrombus formation that
can occlude the coronary tree. |
| Click
to enlarge |
|
Coronary thrombosis is not a simple process. Complex
lesions show multiple complications of the plaque
rupture and erosion, such as healed rupture where
an old rupture is followed by thrombus formation;
the thrombus is organized and the fresh thrombus is
superimposed and the fresh thrombus occludes the coronary
tree (Figure
3).
In the setting of AMI in Japanese patients, former
observations indicated that intimal thickening could
progress to fatal thrombotic occlusion. Vasospasm
may contribute to this process. However, based on
the analysis by Hao and colleagues, fibrocalcific
plaque, which might be stable, could progress to erosion
and cause SCD. Hao ended his presentation, therefore,
with this provocative question: Is “stable plaque”
always calm?
|
PAGE
TOP
|
A
Role for Coronary Angioscopy for the Prevention and
Treatment of Acute Coronary Syndrome
Yasunori Ueda
Osaka Police Hospital, Osaka,
Japan
|
|
Angioscopy is useful for the diagnosis, classification,
risk stratification, and as a treatment guide for
acute coronary syndromes (ACS), and for the evaluation
of drug effects to prevent ACS events.
|
|
Diagnosis and classification using angioscopy
Angioscopy is a useful device to detect the ACS
lesion, usually characterized by yellow plaque and
thrombus. Angioscopy can be used to classify rupture,
erosion, or vasospasm in ACS. Angioscopic classification
of plaque rupture is a large disruption with visible
protrusion, and plaque erosion a small disruption
without visible protrusion of the lipid core. Vasospasm
is characterized angioscopically by the lack of yellow
plaque and only smooth white normal coronary artery,
normal coronary vessel wall, and no adherent thrombus.
In the setting of ruptured plaque, much thrombus
and lipid material is washed away into the distal
circulation system, which may cause microembolization.
Distal protection devices can collect this microembolization
material.
Plaque rupture is also associated with a higher
amount of thrombus, demonstrated by the higher concentration
of TAT in the coronary artery distal from the culprit
lesion. The type of plaque disruption is associated
with infarct size, evaluated by peak-CK, TI-SPECT,
left ventricular ejection fraction (LVEF), and ST
resolution. In the rupture type, the infarct size
is larger and has a higher restenosis rate.
|
|
Risk stratification by angioscopy
|
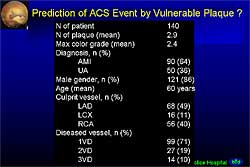 |
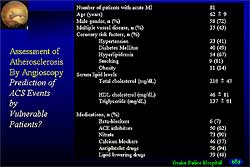
| Figure
1. Characteristics in 140 patients assessed to
predict future ACS based on the presence of vulnerable
plaque. |
| Click
to enlarge |
 |
| Figure
2. Disposition of 81 patients assessed to predict
acute coronary syndrome events. |
| Click
to enlarge |
|
Risk stratification of plaque and the patient can
be performed used angioscopy. As plaque progresses
from stable to vulnerable, it progresses from white
to intensely yellow, with the greater intensity in
the yellow color associated with an increasingly larger
lipid core and thinner fibrous cap. Ueda and colleagues
classified the color of the plaque into 4 grades,
Grade 0 being white and Grades 1, 2, and 3 being progressively
more intensely yellow. The higher the grade the more
thrombus is present. The presence of thrombus means
plaque disruption, so the higher grade is associated
with higher plaque vulnerability. The higher yellow
color intensity of the plaque is associated with a
higher prevalence of positive remodeling; Grade 1
was associated with 10% prevalence, Grade 2 with 30%,
and Grade 3 with 70% remodeling, in their experience.
Therefore, they believe the plaque becomes more and
more yellow, and finally disrupts and causes thrombosis.
However, not all thrombosed plaques cause ACS. Most
thrombosis disruption occurs silently. In 140 patients,
the mean number of yellow plaques was 2.9, and the
average maximum color grade was 2.4 (Figure
1). However, 18 patients suffered a second ACS
event, 3 of whom had undergone angioscopy observation
of the culprit lesion before the second event. Using
angioscopy, determining which plaque may cause a future
ACS event is difficult.
However, an MI patient is a vulnerable patient,
meaning they have many vulnerable plaques. Although
which plaque may cause a future ACS can not be identified,
the presence of many plaques with higher yellow intensity
may be associated with a higher probability of a future
ACS event. Therefore, they tried to validate the extent
of atherosclerosis by angioscopy using these parameters:
number of yellow plaques, maximum color grade, sum
of color grade, and plaque index (number of plaque
multiplied by the maximum color grade).
These parameters were higher in the patients with
a history of MI, compared with patients without a
history of MI, and were also higher in patients with
AMI compared to patients with unstable angina.
They hypothesized the progression of coronary atherosclerosis
as: Yellow plaques develop in the left coronary artery
(LCA), left circumflex (LCx), and left anterior descending
(LAD), some of which cause disruption and thrombosis
and is asymptomatic. The organization of the thrombus
may cause the progression of stenosis, which may lead
to stable angina. However, the disruption of the plaque
in more advanced stages may cause unstable angina.
In more advanced stages, the disruption of the plaque
will cause AMI.
They followed 81 patients who suffered their first
MI for about 5 years, 8 of whom suffered a second
ACS event (Figure
2). The baseline plaque index of these 8 patients
was divided into 2 groups. The patients with a higher
plaque index (>10) had a higher incidence of an
ACS event compared to a lower plaque index (10) [28.6%
vs 4.3%, p=0.02; Figure
3]. Therefore, they believe it is possible to
evaluate the risk of a second ACS event by counting
the number of yellow plaques or evaluating the yellow
color intensity of the plaques, on angioscopy.
|
|
Evaluation of plaque stabilization
It is possible to evaluate the plaque stabilization
by counting the number of yellow plaques or evaluating
the yellow color intensity, which can show the drug
effect. This group evaluated the effect of probucol
(500 mg/day) and found that the drug regresses the
yellow plaque and the lesion becomes white after 1-year
of administration. They are now evaluating this with
statins.
|
|
Evaluation of PCI devices
PCI devices, such as drug-eluting stents, can be
evaluated by angioscopy. For example, at 3 months
after implantation of a bare metal stent, neointima
can be seen covering the stent and the yellow plaques.
It is possible that the neointima reduces the possibility
of a second ACS event at that site. In the natural
course of neointima formation, the neointima becomes
thinner over time, as shown by angioscopy at 3 years.
This group will use angioscopy to study DES and
evaluate the natural course for neointimal coverage
and how long thrombosis will continue. This data will
help to determine the length of time the antiplatelet
drugs should be continued after implantation.
Distal protection devices are used to prevent microembolization
and reduce slow flow and infarct size. Stent thrombosis
is another important problem when treating ACS. Ueda
and colleagues believe this is actually a highly thrombogenic
culprit lesion. To prevent re-thrombosis of the lesion,
it is thought that removal of the disrupted plaque
is needed. Although the frequency is low, re-thrombosis
of the culprit lesion can be fatal. Angioscopy-guided
PCI would be beneficial for removal of the debris.
|
PAGE
TOP
|
Aggressive
Lipid-Lowering Therapy for Secondary Prevention in
Patients with Acute Coronary Syndrome: Volumetric
and Echogenicity Analysis Using Intravascular Ultrasound
Tadateru Takayama
Nihon University School of Medicine,
Tokyo, Japan
|
|
Intensive lipid-lowering therapy for the secondary
prevention of cardiac events is based on data from
several studies, including the findings that plaque
rupture occurs in patients with stable angina or no
symptoms, not just patients with MI or unstable angina,
multiple plaque ruptures may occur in a patient, and
ruptured plaques are eccentric with positive remodeling.
In acute coronary syndrome (ACS), Asakura and colleagues
have shown that a potentially vulnerable plaque was
observed with equal frequency in the infarct-related
and non-infarct-related artery. In other data, multiple
ruptures were observed in 15% of patients.
Vulnerable plaques are frequently observed by intravascular
ultrasound (IVUS) both in the area adjacent to the
culprit lesion and in the non-culprit vessel in patients
with acute coronary syndrome. On IVUS, the vulnerable
plaque is characterized by eccentric, low echogenic
plaque with lipid pool and thin fibrous cap, and positive
remodeling. Typical findings on angioscopy are yellow
plaque, thrombus, and ulceration or erosion.
Randomized clinical trials have demonstrated effective
lipid lowering with a statin in patients with ACS,
and the reduction of primary coronary events, and
reduction of events in patients with stable coronary
artery disease (CAD).
|
|
Study design
To study the effect of aggressive LDL-cholesterol
(LDL-C) lowering on changes in plaque volume and echogenicity
on IVUS, Takayama and colleagues conducted a study
comparing therapy with atorvastatin with or without
anti-oxidant therapy with probucol. Group A
was given atorvastatin 10mg/day, Group P probucol
500mg/day, and Group A+P atorvastatin and probucol.
Inclusion criteria were patients with ACS and non-culprit
lesions, and mild to moderate lesions (< 50% on
QCA). The targets for LDL-C were defined as: LDL-C
³ 140 mg/dl in Group A, < 140 mg/dl in Group P,
and ³ 140 mg/dl in Group A+P.
Baseline and follow-up studies (> 6 months) were
performed with coronary angiogram (CAG) and IVUS (volumetric
and densitometric analysis).
IVUS analysis was performed using 30 MHz Ultracross
or 40MHz Atlantis (Boston Scientific Scimed Inc.),
with an automatic motor drive unit and pull-back speed
at 0.5mm/sec. Off-line volumetric IVUS analysis was
performed to measure lumen volume, vessel volume,
and plaque volume.
Plaque intensity was also determined using Texture
Videodensitometric Analysis. Contrast time investigation
analyzed the change of contrast (gray values) in a
sequence of IVUS images. Gray scales (between black
and white) were divided into 256 values, allowing
regions of interest (ROI) to be defined. The gray
value was measured in the ROI in both plaque
and adventitia.
|
|
Study Results
At 6 months, the total cholesterol level was reduced
in Group A from 228 mg/dl to 147.1 mg/dl, in Group
P from 207 mg/dl to 158 mg/dl, and in Group A+P from
233 mg/dl to 140.4 mg/dl; p< 0.05 for each group.
LDL-C levels was reduced in Group A from 149.4 mg/dl
to 88.8 mg/dl, in Group P from 138 mg/dl to 99 mg/dl,
and in Group A+P from 160.7 mg/dl to 82.3 mg/dl; p<
0.05 for each group.
Only Group A+P had a significant decrease (about
65%) in atheroma volume on volumetric IVUS analysis
from baseline to 6 months (p<0.05). The decrease
in Group A was about 15% and about 20% in Group P.
Lumen volume was significantly increased only in Group
A+P, by about 80% (p<0.05), compared to about 40%
in both Group A and Group P. Vessel volume was the
same, at about 1.0, in each group.
Plaque echogenicity significantly increased in Group
P and Group A+P. However, the increase was greater
in Group A+P (about 90%) than in Group P (about 30%),
each p<0.05 against baseline. On CAG, no significant
change was seen at 6 months in Group A+P.
Before treatment IVUS revealed lipid pools with
an eccentric soft plaque and positive remodeling.
At 6 months, in Group A+P the LDL-C was significantly
decreased from 146 mg/dl to 65.3mg/dl, and IVUS revealed
that the plaque area decreased and the lipid pool
disappeared. In a 67-year-old male patient, the mean
gray value of the plaque increased from 52 to 65.3.
In this patient, the 3D-IVUS measurements showed a
reduction in plaque volume and increase in lumen volume,
indicating plaque regression.
Combination therapy of atorvastatin and probucol regressed
and stabilized the plaque.
In summary, a significant reduction in plaque volume
with a concomitant increase in lumen volume was obtained
in Group A+P. An increase in echogenicity on videodensitometric
analysis was seen in each group but was greatest in
Group A+P.
|
|
Conclusions
Plaque stabilization and plaque regression could
be assessed as changes in plaque volume or echo-intensity
by IVUS. Aggressive lipid-lowering therapy may lead
to plaque regression and stabilization of minor lesions,
which potentially could cause a second cardiac event.
Improvements in tissue characterization on IVUS images
are anticipated with improved equipment for analysis.
|
PAGE
TOP
|
Long-Term
Management of Japanese patients with Coronary Artery
Disease in the Recent Coronary Revascularization Era
for Prevention of ACS
Masatoshi Kawana
Tokyo WomenĦs Medical University,
Tokyo, Japan
|
|
The Heart Institute of Japan (HIJC) group was organized
in 1998 by 17 cardiology centers across Japan, who
agreed to share common diagnostic and therapeutic
strategies with several independent committees, such
as endpoint classification and data and safety monitoring.
Data from HIJC studies presented here showed that
the long-term prognosis of Japanese patients after
acute myocardial infarction (AMI) is better compared
to that in patients in US and European trials. Diabetes
and hypertension are independent risk factors for
morbidity and mortality in Japanese patients. Serum
CRP concentration is a strong and independent predictor
of risk for morbidity and mortality. The incidence
of combined cardiovascular (CV) events was lower in
patients treated with aspirin and statins. However,
patients treated with nitrates and beta-blockers showed
a higher incidence of CV events. In patients without
MI, treatment with a calcium channel blocker (CCB)
resulted in a lower incidence of CV events
|
|
The JAMI study
The HIJC investigated in 3 clinical studies the
long-term outcomes of coronary artery disease (CAD)
in Japanese patients. The endpoints in these studies
were CV events (CV death, non-fatal MI, unstable angina,
heart failure, revascularization), total death, and
CV death.
JAMI was a prospective cohort study to elucidate
the clinical characteristics of AMI in Japanese patients.
A total of 3,021 consecutive AMI patients randomized
within 48 hours of onset in HIJC group hospitals were
included from 1999. The mean age was 68 years, and
80% had ST elevation MI. In contrast to studies conducted
in the US, 54% were smokers.
In contrast to the US and Europe, only 6.5% of the
JAMI patients underwent thrombolysis, while 66% had
primary PCI. Up to 77% of JAMI patients had coronary
revascularization during hospitalization and hospital
CV mortality was 7.9%.
The mean 2.4 years follow-up of 2,736 discharged
patients showed that 57% of patients were on an ACE
inhibitor and 89% on aspirin. The percentage of patients
on a beta-blocker and nitrates, at 32% and 61% respectively,
was higher in Japan compared to clinical trials conducted
in the US and Europe. Patients in JAMI had better
1-year mortality, at 5.7%, than seen in US and European
clinical trials, which ranged from 8.6% to 13.3%.
|
|
The PROCES and CREATE studies
In the prospective cohort PROCES study, designed
to elucidate the long-term prognosis of chronic CAD
in Japanese patients, a total of 2,620 patients with
angiographic evidence of coronary artery lesions were
included in the study. Follow-up information was obtained
from the HIJC registry, and demographic, clinical,
and therapeutic variables were submitted for statistical
analysis to determine the risk factors of adverse
outcomes.
The ongoing CREATE study (Candesartan Randomized
trial for the Evaluation in Coronary Artery Disease)
is a prospective, randomized, open, blinded endpoint
study conducted at HIJC centers. The goal of the study
was to investigate whether the angiotensin receptor
blocker candesartan provides a favorable impact on
prognosis in patients with CAD associated with hypertension.
After confirmation of CAD, including by coronary angiography,
patients were randomized to either candesartan-based
therapy or conventional therapy. The follow-up is
5 years. Patient randomization (n=2,050) was recently
completed. The primary endpoint is CV events, including
CV death, nonfatal MI, unstable angina, and heart
failure requiring hospitalization.
|
|
Meta-analysis of JAMI and PROCES
|
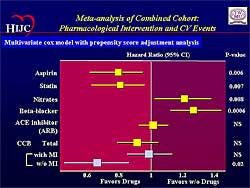 |
| Figure
2. The effect of pharmacologic intervention on
cardiovascular events in the meta-analysis of
the combined cohorts. |
| Click
to enlarge |
|
Kawana and colleagues performed a meta-analysis of
the combined cohort of JAMI and the mid-term analysis
of PROCES. They analyzed the follow-up information
of 5,317 patients with CAD in JAMI (n=2,736) and who
were registered in PROCES. Demographic, clinical,
angiographic, and therapeutic variables were submitted
to statistical analysis to detect the risk factors
of adverse outcomes.
Long-term survival rates at 48 months were significantly
higher at just under 0.9 in patients who underwent
coronary revascularization compared to just over 0.8
in those who did not have revascularization (p<0.0001).
Hypertension and diabetes were independent risk
factors for CV events in the Japanese patients with
CAD, in addition to age and number of diseased vessels
(Figure
1). Hyperlipidemia was not an independent risk
factor, probably because of the prevalence of statin
treatment. Serum CRP was also an independent risk
factor. Patients with CRP in the highest quartile
had a 4-fold risk for total mortality and CV mortality,
and a 2-fold risk for CV events, compared to those
in the lowest quartile. The chronic CAD patients in
the PROCES study in the highest CRP quartile had a
6-fold higher CV mortality. This is the first demonstration
of the impact of CRP as a prognostic marker for stable
CAD in this large number of patients in Japan. These
patients may be candidates for aggressive statin therapy.
The impact of pharmacological interventions for
CV morbidity and mortality was analyzed. The multivariate
Cox model with propensity score adjustment analysis
demonstrated that the incidence of combined CV events
was lower in patients treated with aspirin and statins
(Figure
2). However, patients treated with nitrates showed
a higher incidence of CV events. Surprisingly, patients
treated with beta-blockers also showed a higher incidence
of CV events. Furthermore, in patients without MI,
treatment with a CCB resulted in a lower incidence
of CV events. The Kaplan-Meier curves in CAD patients
without MI showed there was a 38% difference in CV
events between patients treated with a CCB and those
without a CCB. This difference was mainly due to the
reduction of unstable angina requiring hospitalization.
The response to beta-blockers and CCBs seen in the
Japanese patients is quite different from those in
US and European trials. This suggests unique characteristics
in Japanese patients, such as coronary spasm.
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2004
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|