|
|
||||||
|
|||||||
|
|||||||
|
|||
|
|||
Total Arterial Off-Pump CABG in Three-Vessel Disease: SNUH Experience Using Bilateral Internal Thoracic Arteries and Right Gastroepiploic ArteryKi-Bong KimSeoul National University Hospital
|
The advancement of catheter intervention has changed the characteristics of surgical patients. In contrast to just 5 years go, surgical patients are older, with more comorbidities, and poor diastolic volume. The rapid advance of catheter intervention also encouraged cardiac surgeons to address the key limitations of conventional cardiac bypass surgery, such as morbidity of bypass surgery and the consequences of vein graft failure.
Complete arterial off-pump revascularization using skeletonized bilateral internal thoracic arteries (ITA) and right gastroepiploic artery (RGEA) is the current strategy used by Kim and colleagues.
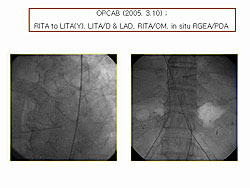
Figures 1 and 2 are from a patient who underwent off-pump coronary artery bypass graft surgery (OPCAB) using the ITA and RGEA. Bilateral ITAs were used to revascularize the left coronary system and the RGEA used to revascularize the PDA. Good patency of the carotids in this patient with very small target vessels was seen on the carotid angiogram taken on the day of surgery.
|
|
Clinical evidence
Two decades ago, Loop demonstrated that saphenous vein grafts (SVG) were associated with a greater risk of death, myocardial infarction (MI), re-hospitalization, re-operation, and cardiac events, compared an ITA graft.
Lytle reported in 2004 the survival of patients who received a single versus bilateral ITA grafts in 1152 propensity-matched pairs. Bilateral ITA grafting improved survival during the second post-operative decade. The two ITAs were undoubtedly the best coronary artery with a 10-year patency rate of more than 90%. The radial and gastroepiploic arteries were the best choices for patients who need 3 or more grafts. From the time that Suma introduced the use of the RGEA in 1987, it has become the conduit most commonly used for bilaterial coronary arteries.
Nishida demonstrated the high early post-operative patency of the ITAs (91-99%) and the RGEA (95%) and the high 5-year survival (92.9%) and cardiac-free survival rate (97.8%) after coronary bypass surgery with only in-situ bilateral ITAs and RGEA.
Tavilla from the Netherlands demonstrated a high 10-year survival rate (87%), and angina-free rate (86%), and cardiac event-free rate (69%) after coronary bypass surgery with only in-situ bilateral ITAs and RGEA.
Experience at Seoul National University Hospital
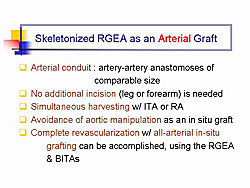
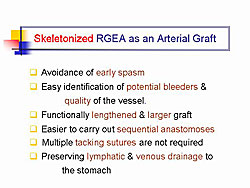
Based on these data, Kim and colleagues used the bilateral ITA and the RGEA for revascularizing patients with 3-vessel disease. The RGEA has several advantages (Figures 3 and 4).
|
|
Limitations of the skeletonized RGEA as an arterial graft include the tendency for vasospasm as a muscular artery; flow competition as been reported when the RGEA has been anastomosed onto coronary artery with a less critical lesion; and hesitation to open the abdominal cavity during cardiac surgery because it may cause complications such as ileus, incisional hernia, or abdominal organ damage.
From January 2000 to December 2004, 676 cases of OPCAB were performed at the Seoul National University Hospital. Of these, 162 cases were 3-vessel disease, requiring ≥4 grafts; BITA and RGEA were used for 132 cases (81.5%), and other grafts were used in the remaining 30 cases.
The mean age of the patients was 62 years, and 31 were women. Nearly one-half had diabetes, one-third had associated left main disease, most patients had unstable angina, and urgent/emergent surgery was performed in 18 patients.
|
Before surgery, evaluation of the arterial grafts was performed using thoracic and abdominal aortography during coronary angiography or thoracoabdominal CT angiography. It is recommended that the RGEA not be anastomosed onto a coronary artery with a less critical lesion, because flow competition inside the right coronary artery has been reported. In addition, if a significant narrowing of the celiac axis was found on the pre-operative aortogram, the RGEA was used as a composite Y-graft or free graft, instead of in-situ graft to avoid the high probability of flow competition.
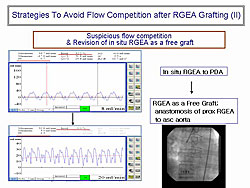
If intra-operative flow measurement suggested a competitive flow pattern, the RGEA was used as a composite graft or free graft instead of an in-situ graft. In one case, intra-operative flow measurement of the in-situ RGEA grafted to the PDA suggested a competitive flow pattern (Figure 5). Kim and colleagues divided the RGEA at the proximal section and it was anastomosed to the ascending aorta. The subsequent flow measurement suggested a successful outcome, and the post-operative angiogram showed a good patency.
A standard skeletonizing technique for harvesting the ITA and RGEA was used in all cases. The bilateral ITA to revascularize the left coronary system and the RGEA for the right coronary system was used.
The types and number of grafts used in the 132 cases at SNUH.
|
*4/0 were in-situ plus composite graft with a segment of RGEA
An average of 4.2 anastomoses were used per patient. There was 1 early operative death and 1 late (> 30 days) death. The ICU stay was 26 hours on average and the hospital days were 9 on average. The post-operative morbidity was:
|
Coronary angiography was performed in 130 patients within 1.3 days post-operatively, and the post-op patency rate was 99.3% for ITA and 97.9% for RGEA (NS).
In conclusion, total arterial OPCAB using bilateral ITAs and RGEA could be performed in nearly all patients requiring ≥4 grafts. Skeletonized RGEA is excellent as a third arterial graft in terms of early patency and clinical outcomes.
Alcohol Septal Ablation Therapy in Hypertrophic Obstructive CardiomyopathyCheol Whan LeeAsan Medical Center
|
Left ventricular outflow obstruction (LVOT) is an important mechanism for symptom production in hypertrophic obstructive cardiomyopathy (HOCM). Therapies that reduce LVOT pressure gradient, such as surgical myectomy, pacemaker, alcohol septal ablation therapy (AST), may improve LV filling pressure and clinical symptoms.
Advantages of AST include nonsurgical technique for septal myocardial reduction, and dramatic hemodynamic improvement. Further, the technique is technically easy for most interventional cardiologists. Therefore, it has been increasingly used, especially for HOCM refractory to medical therapy. However, limitations include potential serious complications (large infarction, complete AV block requiring pacemaker, and ventricular tachyarrhythmia). Further, the therapeutic benefit is not maintained in all patients, with eventual recurrence of LVOT pressure gradient.
Lee and colleagues previously reported that the therapeutic benefit is maintained in most patients. However, in some patients LVOT pressure gradient was significantly recovered during the follow-up, despite the early successful result. There is little data about the incidence and determinants of hemodynamic recurrence after successful procedures.
Study of AST at Asan Medical Center
|
Thus, Lee and colleagues conducted a study to investigate the incidence and determinants of hemodynamic recurrence after successful AST, and the relation between ethanol dose and its impact on hemodynamic and clinical outcomes. The indications for AST are shown in Figure 1.
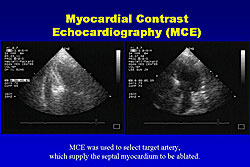
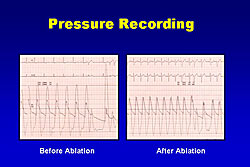
Between December 1996 and March 2004, 37 patients (20 women, 17 men) with symptomatic HOCM underwent AST at the Asan Medical Center. All patients received a temporary pacemaker, and an angioplasty balloon (1.5 – 2.5 mm) was positioned at the proximal portion of the septal artery, and myocardial contrast echocardiography (MCE) was used for proper localization and quantification of the septal infarction after the enthanol injection. Absolute alcohol (usually 2-3 ml) was slowly injected through the lumen of the inflated balloon into the septal artery and left for 5 minutes before the balloon was deflated. Figure 2 shows the MCE from one patient. A typical pressure recording from these patients shows that the LV pressure gradient are usually dramatically reduced immediately nearly to zero (Figure 3).
|
|
After AST, all patients were observed in the intensive care unit for 1-3 days. ECG and cardiac enzymes were carefully monitored, and patients were usually discharged 7 days after AST.
In this study, the target artery was the 1st septal branch in 31 (81%) of patients, and the 2nd septal branch in 6 (16%) of patients. The amount of alcohol used was 3.7 ± 2.1ml, and MCE was used in the last 16 cases. Clinical follow-up was performed every 3 months and echocardiographic follow-up was performed before surgery, and 3-6 months and 1 year after surgery.
A high 95% (35 of 37 patients) procedural success was achieved, defined as the relief of symptoms and the reduction of LVOT pressure gradient >50% of baseline in the catheterization lab. Symptomatic improvements (NYHA class ≥ grade 1) was achieved in 31 of 25 patients (88% success).
|
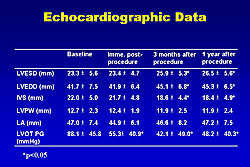
The echocardiographic data obtained in the 37 patients is shown in Figure 4. LV end diastolic and systolic dimensions were slightly increased during the follow-up. IVS was significantly decreased during follow-up.
Serial changes in LVOT measured by echocardiogram showed that it was remarkable reduced from 88 to 55 immediately after the surgery and this reduction was maintained at 2 years in most patients. However, in some patients the LVOT was significantly recovered at AST (9 patients in hospital, 2 patients at 6 months, 3 patients at 1 year). Thus, they defined hemodynamic recurrence as a re-elevation of LVOT pressure ≥50% of baseline after a successful procedure. Of 35 patients with successful procedure, 14 patients (40%) had recurrence of LVOT obstruction.
|
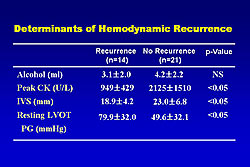
There were no differences between the recurrence and non-recurrence groups for age, follow-up duration, initial NYHA functional class, and use of MCE. NYHA class at follow-up tended to be better in the non-recurrence group, but this did not achieve statistical significance. Peak CK level and IVS were significantly higher in the non-recurrence group and resting LVOT was significantly higher in the recurrence group (Figure 5). A lower CK level (<1,100 U/L) was the only independent determinant of hemodynamic recurrence (OR 27.7, p<0.05, 95%CI 1.9-403.1). The peak CK level was significantly correlated with the alcohol dose.
Early complications included death in 1 (3%) patient, LAD infarct in 2 (5%) patients, permanent complete AVB in 5 (14%) and transient CAVB in 18 (49%) patients. Late complications included death in 4 patients (2 cardiac, 2 non-cardiac).
Predictors of major complications (cardiac death, LAD infarction, CAVB) were a peak CK level > 2,000 U/L (50.0% vs. 22.2%, p<0.05) and the amount of alcohol ≥4ml (70.0% vs. 25.9%, p<0.05). The amount of alcohol injection≥4ml was an independent determinant of major complications (OR 15.33, 95% CI : 1.53-163.55, p<0.05)
In conclusion, AST is a promising non-surgical technique for septal myocardial reduction in HOCM. However, major complications remain a serious problem, which were primarily related to the large amount of alcohol injected (<4 ml). Further, hemodynamic recurrence may be an important limitation of AST, which was related to insufficient infarction. The target artery and ethanol dose (2-3 ml) should be carefully selected obtain therapeutic benefits without major complications.
|
|
| Copyright © 2005 Japanese Circulation Society All Rights Reserved. webmaster@j-circ.or.jp |