|
|
||||||
|
|||||||
|
|||||||
|
|||
|
|||
Circulating Progenitor Cell as an Endothelial Functional MarkerYasushi NumaguchiNagoya University School of Medicine
|
Novel, emerging risk factors for endothelial damage include hyperhomocysteinemia, obesity, physical inactivity, postprandial state, and chronic inflammation. Additional contributors to endothelial dysfunction are genes, intrinsic susceptibility and the environment. Endothelial progenitor cells (EPCs) have been shown to maintain vascular function in middle-aged and older-aged persons with coronary risk factors, as well as a correlation between cluster formation of EPCs and risk factors.
Numaguchi and colleagues from Nagoya University School of Medicine sought to determine whether the same relation between EPCs and endothelial function exists in young healthy subjects without overt coronary risk factors. This relationship, if present, would be useful for identifying endothelial dysfunction, thereby allowing for the prevention of atherosclerosis and disease progression.
In the present study, they analyzed the relation between functional characteristics of EPCs and endothelial function, and examined the effects of smoking on the behavior and function of EPCs. Smoking is the most serious risk factor in the young male Japanese population, and cardiovascular disease from smoking is increasing in this population.
The mechanism of EPC entrapment into the vascular wall was evaluated as a measure of EPC function, and three stages were studied: mobilization, attachment and migration, and differentiation.
In the 88 male volunteers (33±6 years old, range 25-29), the baseline characteristics were within the normal range, with no hypertension or dyslipidemia. No relation was found between the lipid profile, insulin resistance, and concentration of growth factors and flow-mediated dilation (FMD).
A positive correlation between the level of ICAM-1 (ρ=0.349, p=0.018) and VCAM-1 (ρ=0.426, p=0.029) with the rate of cell attachment to mononuclear cell (MNC) count was found, but no correlation with the differentiation index as defined as the ratio of EPCs to the number of attached cells.
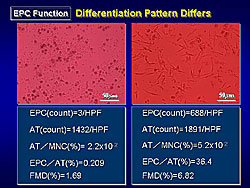
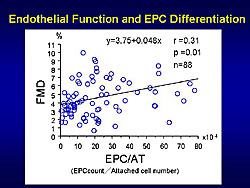
Notably, they found that the differentiation patterns were different between subjects, with the non-round shape in some subjects suggesting the EPCs were differentiating to endothelial lineage cells (Figure 1). EPC differentiation reflects endothelial function even in young healthy subjects, as shown by the moderate correlation that was found between the differentiation index and FMD (Figure 2).
|
|
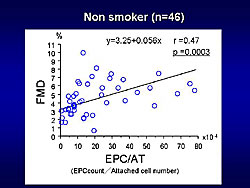
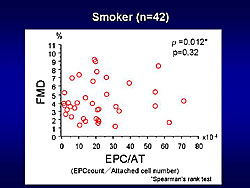
Smoking inhibited EPC attachment and smoking cessation increased the mobilization and attachment of EPCs, in this comparison of 42 smokers and 46 nonsmokers (Figures 3 and 4). The smokers and nonsmokers were comparable, except for folic acid levels (8.8 ng/ml in nonsmokers, 6.2 ng/ml in smokers; p=0.017) and homocysteine levels (10 nM/mL nonsmokers, 12nM/mL smokers; p=0.29).
In conclusion, these investigators state that the correlation between EPC differentiation to endothelial cells and the degree of endothelial function may be a novel early marker of arteriosclerosis.
|
|
Clinical Importance of Endothelial Function Testing in Cardiovascular DiseaseAndreas M. ZeiherUniversity of Frankfurt
|
A good vasodilatory response to increased blood flow, after a vasodilator was injected into the artery, was associated with the lowest risk of major cardiovascular events (MACE), while a poor dilatory response, suggesting an impairment in nitric oxide (NO) release, had the highest MACE risk, as shown by a 10-year study conducted by Park and colleagues.
|
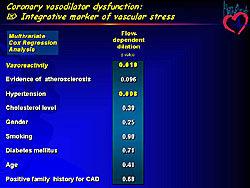
Vasodilatory function, which is endothelium-dependent, may be an integrative marker of vascular stress, as shown on multivariate analysis. Only vasodilatory function and hypertension remained independent predictors of further events (Figure 1). Coronary and peripheral endothelial dysfunction significantly predict future MACE, according to more than ten published studies; this suggests that endothelial dysfunction is an independent predictor of future adverse events in patients at risk or with stable coronary artery disease (CAD).
These studies provide clinical confirmation of the hypothesis that systemic risk factors interfere with the balance between NO and other endothelium-derived protective mediators and superoxide production that leads to an inflammation of the endothelium, a process called endothelial activation, which alters the milieu in the vascular wall, leading to cytokine production, redox-sensitive gene expression and apoptosis—the basis for the development of plaque, and its inflammation and vulnerability.
Atherosclerosis is a chronically low-grade inflammatory disease of the vascular wall, and both inflammation and endothelial activation are mediators of disease progression. This concept has led to the hypothesis that risk factors will act on the vascular wall, produce cytokines that act directly on the vascular wall and also on the liver to produce C-reactive protein (CRP) as an acute phase reactant, and this scenario will eventually lead to the occurrence of an acute coronary syndrome (ACS). High-sensitivity CRP (hsCRP) is a marker produced by the liver that reflects the inflammatory state.
Zeiher and colleagues showed that in patients with CAD, by measuring endothelial function in the forearm circulation, there are low levels of CRP, a well-preserved vasodilatory response to the infusion of acetylcholine, and that the vasodilatory response is blunted if there are elevated levels of CRP.
Vulnerable plaque or vulnerable patient?
An increase in CRP levels, even in the presence of low LDL levels, is associated with MACE, suggesting that they are both markers of endothelial inflammation. Thus, Zeiher stated, this leads to the questions: Is there actually vulnerable plaque, or is there a vulnerable patient harboring vulnerable plaques?
To address these questions, they assessed the endothelial function in the systemic circulation. Zeiher and colleagues showed reduced vasodilatory responses to acetylcholine in the forearm circulation in patients who suffered a second ACS event, compared to those who did not.
These investigators also showed that patients with the best endothelium-dependent vasodilatory response (in the highest quartile) had the least events over 5 years compared to those with evidence of a systemically-impaired endothelium-dependent vasodilation (n the lowest quartile), based on measurements of forearm blood flow.
On multivariate analysis, only systemic endothelial vasodilator function and troponin, a classic marker of myocardial necrosis in ACS, predict future events in ACS survivors.
In patients who spontaneously recover endothelial function over time, their acetylcholine-mediated FBF response is significantly improved, compared to patients having further events over time. The patients with the best spontaneous recovery of endothelial function after an ACS had the best event-free survival, while those with an impaired vasodilatory response to acetylcholine 4 weeks after an ACS had the most future events.
Thus, impaired endothelial function of the forearm is associated with further CV events in patients who survived an ACS episode. Systemic endothelial vasodilatory capacity provides additional information compared to classical risk factors or classical markers, like CRP or troponin. The spontaneous improvement of systemic vasodilator function over time is associated with a reduction of CV events. Zeiher stated that these data provide unequivocal evidence for the existence of the vulnerable patient, rather than the vulnerable plaque. Further, that this type of assessment might provide an integrated index of systemic inflammatory activation of the vascular wall, and thus enable the identification of the inflamed vulnerable patients.
Identifying vasoprotective mechanisms
Endothelial activation seems to reflect risk factor actions, such as cytokine inflammation, and therefore, it should be possible to use this technique to identify vasoprotective mechanisms, for example ACE inhibitors, statins or endothelial progenitor cell (EPCs) effects.
Assessing the vascular phenotype, using a minimally invasive strategy, may provide an integrated index of systemic inflammatory activation of the vascular wall, and, thus, enable the identification of the inflamed “vulnerable” patient at risk.By antagonizing TNF-alpha, an inflammatory mediator, with a TNF-alpha receptor blocker, these investigators showed a significant improvement in systemic endothelial vasodilator function, which returned to the impaired level 7 days later.
The additive effects between LDL cholesterol levels and CRP levels are well known. In the PROVE-IT trial, when CPR was lowered below a specified threshold, it remained associated with an improvement in events, whether or not LDL levels were lowered below 70 mg/dL. This can be mirrored when looking at endothelial vasodilator measurements. The patients who had greater than the median reductions in CRP and LDL had the best improvement in vasodilatory function of the forearm circulation, and those who did not respond to both parameters had the least responses.
Therefore, these improvements are thought to be the result of EPCs repairing denuded areas of the vascular wall. Thus, the balance between endothelial injury and endothelial regeneration may reflect the healthiness or the functional integrity of the endothelium.
This concept is supported by data from Hill and colleagues, showing endothelial flow-dependent vasodilation was correlated with the colony-forming capacity of the repair cells. The repair cells are mobilized by statins, as shown by Vasa and colleagues. The number of circulating EPCs predict future outcome. Elevated levels of CD34-positive cells is associated with nearly no events, while a low level is associated with the occurrence of events over time. This suggests there is a balance between endothelial injury and endothelial repair that determines the outcome of patients.
Routine clinical testing of endothelial function?
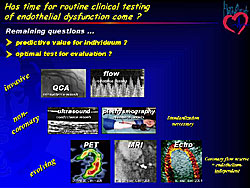
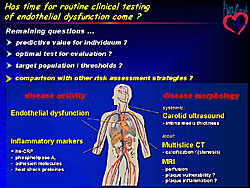
Has the time come for routine clinical testing? There is clear proof of concept that measuring endothelial dysfunction provides pathophysiologic insights. The predictive value is unknown, as well as the optimal test to use, or whether testing should be invasive into the coronary arteries or noninvasive using ultrasound or plethysmography of the peripheral circulation or use evolving techniques (Figure 2). Other unknowns include the target population to test and how the measurement compares to other risk assessments, for example, measuring inflammatory markers or using disease morphology imaging techniques (Figure 3).
|
|
Summary
Testing endothelial function is clinically important because it clearly reflects endothelial activation, which underlies vasomotor dysfunction and also plaque growth and progression. Endothelial activation contributes to acute disease manifestation and is prognostically predictive. It also reflects the repair capacity, for example, as measured by circulating EPCs. This testing is a tool, at least as a surrogate, to assess interventions to improve outcomes in patients, simply by looking at endothelial vasodilator function.
Vascular Dysfunction is a Common Finding in Patients with Poor Exercise Capacity and Sympathetic DysfunctionShigeyuki WatanabeGraduate School of Comprehensive Human Sciences
|
Exercise intolerance, sympathetic disturbance, and vascular dysfunction
are reported to increase the risk of death from cardiovascular disease
(CVD). Exercise intolerance may be the strongest predictor of an
unfavorable prognosis in unhealthy subjects and in patients with
CVD. However, the relationship between these indices is unknown.
This group hypothesized that vascular function and sympathetic nerve activity are involved in determining the exercise intolerance through the skeletal muscle vasodilation during exercise. The objectives of the present studies were to determine whether vascular function is related to exercise capacity and whether vascular function is related to sympathetic dysfunction.
The noninvasive evaluation of working muscle vasodilation (exercise hyperemia) has proven difficult. Near infrared spectroscopy (NIRS) is a noninvasive method to measure tissue hemoglobin content. It was previously shown that total hemoglobin (total Hb) increased with exercise, and this also represents a change in blood volume. Hence they hypothesized that changes in working muscle total Hb indicates muscle vasodilation was conductance of the vessel.
They studied this hypothesis in 10 cardiac patients, who performed symptom-limited, incremental bicycle exercise testing; using a 5 Fr Swanz-Ganz catheter to measure common iliac vein and femoral-venous blood flow every minute during exercise. Conductance was calculated as blood flow divided by mean blood pressure. Changes of total Hb and leg vessel conductance were strikingly similar during exercise. This concordance between the total Hb and vessel conductance were confirmed in each of the 10 cases. Thus, they used changes in total Hb as an index of muscle vasodilation in the present studies.
Study One
In this study were 23 male patients with ischemic heart disease (61 years, 16 with prior MI and LVEF 41%, 7 patients with angina pectoris).
The patients underwent exercise testing with NIRS measurement, and changes in total Hb was used as an index of muscle vasodilation, and peak oxygen uptake and the anaerobic threshold were indices of exercise capacity. They also underwent strain-gauge venous occlusion plethysmography, with intraarterial administration of acetylcholine or sodium nitroprusside (SNP), and endothelium-dependent and independent vasodilation in the forearm was measured.
Vascular resistance and acetylcholine infusion tended to correlate with the anaerobic threshold, but not with the peak oxygen level. Vascular resistance after infusion of SNP was significantly and inversely correlated with anaerobic threshold and peak oxygen level (VO2). This indicates that exercise performance is predominantly related to endothelium independent vasodilation. Vascular resistance under SNP infusion correlated with exercise muscle vasodilation, but there was no correlation under acetylcholine infusion. Muscle vasodilation was significantly correlated with both anaerobic threshold and peak oxygen uptake.
In summary, exercise tolerance was closely related to exercise-induced muscle vasodilation. Both exercise tolerance and exercise-induced muscle vasodilation are related to endothelium-dependent vasodilation and predominantly to endothelium-independent vasodilation in cardiac patients.
Study Two
In this study were 24 male patients with heart disease (59 years, 13 with MI and LVEF 41%, 4 with angina pectoris, and 7 with dilated cardiomyopathy with an LVEF 51%).
The patients underwent cardiopulmonary exercise testing with NIRS measurement, and cardiac MIBG study, as an index of sympathetic nerve activity. Also, skeletal muscle MIBG study was performed to evaluate the sympathetic nerve activity of the skeletal muscle. Endothelium-dependent and independent vasodilation in the forearm and reactive hyperemia flow were evaluated.
Late phase heart to media ratio of MIBG uptake correlated well with the increase in muscle vasodilation and reactive hyperemia. This indicates that preserved H/M ratio is accompanied by preserved exercise tolerance. Vascular MIBG washout inversely correlated with exercise muscle vasodilation and exercise tolerance, suggesting that muscle sympathetic hyperactivity is associated with poor muscle vasodilation and poor exercise tolerance in these patients.
Leg to brain uptake ratio of MIBG correlated well with endothelium-independent vasodilation in the patients with poor exercise capacity, but it did not correlate with endothelium-dependent vasodilation.
In summary, heart sympathetic nerve dysfunction was closely related to muscle vascular dysfunction and poor exercise tolerance. Moreover, muscle sympathetic dysfunction was related to predominantly endothelium-independent vascular dysfunction and exercise intolerance.
Conclusions
Vascular dysfunction, especially impaired muscle vasodilation during exercise, is a common finding in patients with poor exercise capacity and sympathetic dysfunction, and might be an index of the prevention of CVD in the patients with poor exercise capacity.
Moreover, exercise therapy might be a good choice of treatment for the patients with vascular dysfunction
|
|
| Copyright © 2005 Japanese Circulation Society All Rights Reserved. webmaster@j-circ.or.jp |