|
|
|
 |
Congress Report
|
 |
the 70th Scientific Session
|
 |
Joint Symposiums
|
|
|
|
Advanced Cardiovascular Ultrasound
|
|
|
|
|
|
Detection of Postischemic Regional Left Ventricular Delayed Relaxation after Exercise-Induced Ischemia in Patients with Effort Angina Using Diastolic Color Kinesis
Katsuhisa Ishii
Kensai Denryoku Hospital
Osaka, Japan
Regional left ventricular (LV) diastolic dysfunction may persist after systolic function returns following transient severe myocardial ischemia and may be a sensitive indicator that transient severe ischemia has occurred. Dr. Katsuhisa Ishii of Kensai Denryoku Hospital and colleagues used color kinesis (CK) to evaluate regional LV diastolic wall motion following treadmill exercise stress test in patients with exercise-induced angina. The objective of the study was to determine if coronary artery disease can be diagnosed and stenotic coronary arteries identified by detecting post-ischemic regional LV diastolic asynchrony with CK.
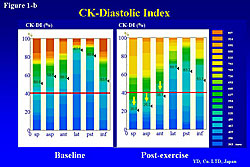
The investigators developed a CK-diastolic index (CK-DI), focusing on the LAD segment and dividing it into two segments: the LV segmental area of expansion during the first 30% of diastole and the LV segmental area of expansion at end-diastole. CK-DI ≤40% was defined as regional LV delayed outward motion during early diastole. Analysis of CK-DI in 36 normal control subjects (20 men, 16 women; 60 ± 4 years) with a mean heart rate of 62 ± 5 beats per minute and mean blood pressure of 132 ± 11 mm Hg showed normal CK-DI values in the following segments: CK-DI (LAD) = 73±6%; CK-DI (LCX) = 78±8%; and CK-DI (RCA) = 70±5%.
CK-DI was determined in 61 patients (51 men, 10 women; 66±9 years) with effort angina (EA) and in 30 normal subjects (20 men, 10 women; 62±7 years). Symptom-limited treadmill exercise testing was performed within one week prior to undergoing diagnostic coronary angiography. CK images were obtained in the short axis and apical views at baseline and 20 minutes after exercise testing, and analyzed with ICK software.
|
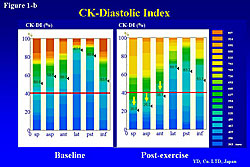
Figure 1. In a 75-year-old man, the color kinesis-diastolic index (CK-DI) decreased significantly after exercise compared to baseline.
Click to enlarge |
|
|
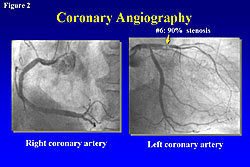
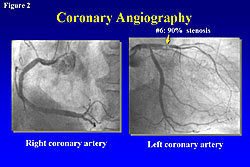
Figure 2. Significant stenosis in the left coronary artery was found in a 75-year-old man in the study.
Click to enlarge |
|
|
Ishii presented a case study of a 75-year-old male with EA enrolled in the study. Analysis of CK performed at baseline and post-exercise stress test showed that the CK-DI decreased significantly after exercise compared to baseline (Figure 1). Coronary angiography showed significant stenosis in the left coronary artery (Figure 2).
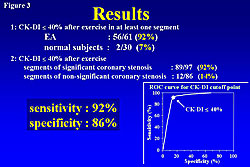
Results showed that 56 (92%) EA patients with normal diastolic wall motion before exercise had new regional LV delayed outward motion during early diastole (CK-DI ≤40%) in at least one segment after exercise testing. Two (7%) normal subjects had CK-DI ≤40% after exercise testing. Coronary angiography showed that 89 of 97 (92%) segments with significant coronary artery stenosis had CK-DI ≤40% after exercise testing. Of 86 segments with non-significant coronary stenosis, 12 (14%) had CK-DI ≤40%. Data analysis showed that this method had 92% sensitivity and 86% specificity (Figure 3).
Ishii concluded that detection of post-ischemic asynchrony using CK after a treadmill exercise stress test may be a sensitive method for the diagnosis of coronary artery disease. |
Advances in Stress Echocardiography
Thomas H. Marwick
University of Queensland
Australia
In nearly two decades of increasing use, stress echocardiography has become a standard clinical tool. Dr. Thomas H. Marwick, University of Queensland, discussed limitations of stress echocardiography and potential solutions stemming from new technologies.
Recent advances in contrast echocardiography have helped improve image quality. A number of studies demonstrated that use of micro-bubbles for left ventricular opacification (LVO) improves endocardial resolution, and a new study showed that this increases the test’s accuracy.
A learning curve is required for accuracy in interpretation—novice echocardiographers have about 60% accuracy, which increases to 80% after six months of experience. Data from Marwick’s lab show that when physicians start doing stress echocardiography, they over-diagnose wall motion abnormalities, causing poor specificity. Additionally, personal training is necessary, as novice echocardiographers did not improve when instructed by CD-ROM. Novice readers’ concordance with expert diagnoses improves with enhanced echocardiography compared to unenhanced images. Novices’ accuracy also improved when they were given the tissue velocity cutoffs. A problem exists with inter-institution agreement because different echocardiographers have different thresholds for pathologic diagnoses. A large multicenter study found that concordance between centers can be improved by using new technologies for quantitation, such as tissue velocity, displacement, or cutoffs.
Sensitivity of stress echocardiography can be limited in patients with small LV cavity size, which can reduce wall stress. A 2003 study found that using a beta blocker immediately after stress causes the LV cavity to enlarge, allowing visualization of wall motion abnormalities, thereby increasing sensitivity.
Marwick’s lab developed a myocardial contrast approach combining exercise with a contrast agent to improve sensitivity. In one example, without the contrast, the LV cavity was reduced in size and no wall motion abnormalities were apparent. When contrast was added, post-stress images showed a subendocardial perfusion defect in the apex. Several other studies confirmed that sensitivity is improved with myocardial contrast on top of wall motion assessment. Recently published data from Marwick’s lab show that strain rate imaging (SRI) has the same sensitivity and specificity as an expert observer.
Marwick concluded that the standard wall motion approach is good for accuracy, prognostic value, and detection of viable myocardium. However, it is vitally important to keep attending to adequate training. Using myocardial contrast and TDI/strain may improve subjectivity and the learning curve. Contrast may particularly help with mild disease, recognition of multivessel disease, and ischemia within areas of resting wall motion abnormality. The challenge will be to maintain the high feasibility and low cost of this test. The new technologies should be applied carefully so that analysis time and cost are not increased. |
Tissue Doppler Echocardiographic Evaluation of Cardiac Function
Katsu Takenaka
University of Tokyo
Tokyo, Japan
Regional myocardial strain is an index of regional myocardial function that can be measured by either tissue Doppler ultrasound or two-dimensional tracking.
Professor Katsu Takenaka, University of Tokyo, described his studies of myocardial strain measurements for diagnosing myocardial ischemia and other conditions.
|
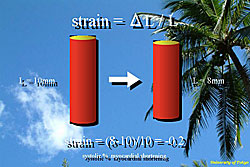
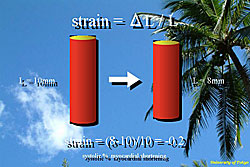
Figure 1. Myocardial strain is measured by the change in the length of the segment (ΔL) over the segment length (L), and corresponds to the systolic percent myocardial shortening.
Click to enlarge |
|
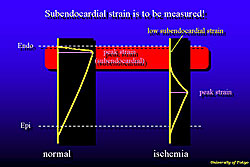
Myocardial contraction is not homogeneous throughout the heart, as evidenced by higher strain in the subendocardial region than in the subepicardial region. Myocardial strain is measured by the change in the length of the segment (ΔL) over the segment length (L) (Figure 1). This measurement corresponds to the systolic percent myocardial shortening.
The normal LV posterior wall is 10 mm thick and increases to 16 mm at end systole, a 60% systolic strain. The ventricle is composed of three or four thin myocardial layers, each with fibers running in different directions and connected by a loose collagen network. The sheets curve steeply as they approach the endocardium and with each contraction slide over one another, becoming steeper and pushing the endocardium towards the left ventricular (LV) cavity. Thus, the 60% systolic wall thickening is achieved by rearrangement of the subendocardial sheets, while each myocardial cell only thickens 8%.
|
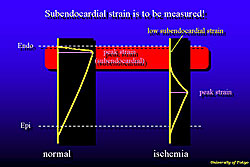
Figure 2. In normal subjects, peak strain occurs in the subendocardial myocardium, then gradually decreases toward the epicardium.
Click to enlarge |
|
|
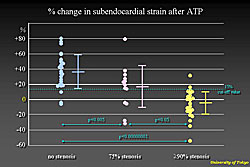
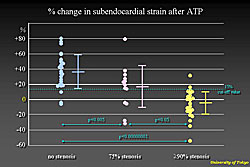
Figure 3. Subendocardial strain after ATP infusion increased 35% in segments without stenosis, 18% in segments with 75% stenosis, and did not increase or decrease in segments with severe stenosis.
Click to enlarge |
|
Regional strain is calculated and displayed using tissue Doppler data, on the assumption that every segment contracts towards the center of the LV wall. In normal subjects, peak strain occurs in the subendocardial myocardium, then gradually decreases toward the epicardium (Figure 2). In ischemic myocardium, the dynamic range of subendocardial strain value is very wide from the normal to the pathological state. Therefore subendothelial strain should be measured instead of the percent of wall thickening or endocardial excursion.
ATP increases coronary flow two- or three-fold in normal myocardium. Distal to a significant stenosis, ATP fails to increase blood supply. However, augmented contraction during ATP infusion in the normal myocardium can be identified by the strain measurement method. Subendocardial strain after ATP infusion increased 35% in segments without stenosis, 18% in segments with 75% stenosis, and did not increase or decrease in segments with severe stenosis (Figure 3). Using a 15% increase in strain as the cutoff value, ROC curve showed that this method can make a diagnosis of more than 90% stenosis with 94% sensitivity and 83% specificity.
Additionally, subendocardial strain measurement using TDI was used to diagnose dose-dependent myocardial damage caused by anthracycline. Dr. Takenaka concluded that subendocardial strain measurement can be used to diagnose a variety of pathological states. |
|