|
|
||||||
|
|||||||
|
|||||||
|
|||
|
|||
Surgical Treatment of FMR in the Patients with LVEF ≤ 40% – Early and Mid-Term ResultsRyuzo SakataDepartment of Thoracic Cardiovascular Surgery, Kagoshima University, Kagoshima, JapanCurrent surgical approaches for functional mitral regurgitation (FMR) primarily focus on reshaping the annulus by ring annuloplasty (MAP). However, many patients have persistent or recurrent FMR after MAP. Ryuzo Sakata, MD, Kagoshima University, presented results of a study on the surgical strategy used at Kagoshima University. At Kagoshima University, patients with FMR are treated with MAP, MAP and left ventricular plasty (LVP), or MAP and LVP plus subvalvular procedures, depending on the cause and severity of FMR. LVP is done by the Dor procedure, the SAVE procedure, or an overlapping procedure. Three types of subvalvular procedures are used to reduce tethering force: chordal cutting, papillary muscle realignment, or papillary muscle elevation. Out of 80 patients who had operations for FMR in the past 7 years, 52 patients with left ventricular ejection fraction (LVEF) ≤40% were selected for this study. Of these patients, 46 had ischemic MR and 6 had dilated cardiomyopathy (DCM). The mean age was 65, with 19% of patients ≥75 years. Sixteen (31%) patients had multi-territory myocardial infarction (MI). The mean LVEF was 31%, mean LV end-diastolic volume index (LVEDVI) was 103, and the mean MR grade was 1.9. CABG was performed in 44 patients. All 52 patients underwent MAP (29 Carpentier ring, 23 flexible linear reducer). LVP was performed in 33 patients (5 Dor, 10 SAVE, 14 overlapping, 4 other). Subvalvular procedures were performed in 18 patients (9 papillary muscle realignment, 11 chordal cutting, 2 papillary muscle elevation). Additional procedures performed included tricuspid annuloplasty (n=10), Maze (n=5), aortic valve replacement (n=1), ascending aorta replacement (n=2), and biventricular pacing (n=1). Five (9.6%) patients required re-operation and 3 (5.8%) underwent emergency surgery. In the early postoperative period, there were 2 (3.8%) operative deaths (≤30 days), 3 (5.8%) hospital deaths, and 2 (4%) cases with bleeding complications. All early postoperative (1-2 weeks) echocardiographic parameters, except LVDs, were significantly improved after surgery (Slide 20). The mean MR grade was improved from 1.9±1.0 before surgery (n=52) to 0.2±0.4 after surgery (n=50). At the mid-term analysis (33.7 [5-68] months) (n=47), there were 5 (11%) deaths. Actuarial survival at six postoperative years was 80%. Midterm echocardiography results (n-37) showed that the mean MR grade was 0.6±0.7. According to Dr. Sakata, this surgical strategy for FMR provided acceptable early and mid-term outcomes in patients with LVEF ≤40% and had a positive impact on prevention of MR recurrence in the mid-term postoperative period. |
Cardiac Resynchronization Therapy for Heart FailureChun-Chieh WangSecond Section of Cardiology, Chang Gung Memorial Hospital, Tapei, TaiwanApproximately 15% of all patients with chronic heart failure (CHF) and 30% of those with severe CHF have ventricular dyssynchrony, as indicated by prolonged QRS (>120 ms). These patients have a significantly greater risk of death than patients with QRS <120 ms. Chun-Chieh Wang, MD, Chang Gung Memorial Hospital, discussed recent advances in cardiac resynchronization therapy (CRT) for patients with CHF. CRT can improve atrioventricular, intraventricular, and interventricular contraction by atrial synchronous biventricular pacing. AV resynchronization improves mitral regurgitation, while intraventricular and interventricular resynchronization improves left ventricular (LV) mechanical energetics, improves hemodynamics, and promotes LV reverse remodeling.
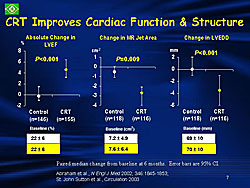
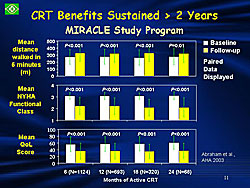
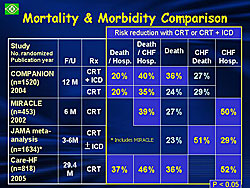
Early CRT trials focused on improving symptoms and quality of life indicators. Current trials are evaluating disease progression, mortality, and morbidity. Two trials in 2002 and 2003 demonstrated that CRT significantly improves left ventricular ejection fraction (LVEF) (P<0.001), reduces mitral regurgitation (MR) (P=0.009), and reduces LV end diastolic diameter (LVEDD) (P<0.001) (Figure 1). The MIRACLE study program, including the MIRACLE, MIRACLE ICD, and InSync III trials, demonstrated improved quality of life (P<0.001), exercise capacity (P=0.01), and NYHA functional class (P<0.001) with two years of active CRT (Figure 2). These trials ended with US Food and Drug Administration (FDA) of the device under evaluation. Results of several studies demonstrated that CRT reduces the risk of death and hospitalization in patients with CHF (Figure 3). The CARE-HF study (n=818) showed conclusively that CRT reduces both morbidity and mortality substantially in patients with symptomatic CHF due to LV systolic dysfunction complicated by dyssynchrony. Calculations suggest that for every 9 devices implanted, 1 death and 3 hospitalizations for major cardiovascular events were prevented. Many patients in this trial also improved symptomatically. CRT consistently improves quality of life, functional status, and exercise capacity. Strong evidence also exists for promotion of reverse modeling with CRT. CRT reduces CHF and all-cause morbidity and mortality. Currently, there are more than 4,000 patients enrolled in randomized, controlled trials of CRT. Dr. Wang concluded that CRT offers an adjunctive approach for treating patients with ventricular dyssynchrony in the setting of moderate to severe CHF. Proper management of CRT patients involves cooperation among the primary care physician, electrophysiologist, echocardiographer, and CHF specialist. With adequate adjustment of AV and VV delay and careful interpretation of pacemaker memory data, including resting heart rate, activity level, heart rate variability, and estimated fluid status for guiding therapy, patients’ symptoms and long-term outcomes can be improved. |
Exercise Training for Chronic Heart FailureAndrew JS CoatsFaculty of Medicine, University of Sidney, AustraliaPhysical activity was restricted for patients with chronic heart failure (CHF) until the 1990s when studies began to show the beneficial effects of exercise. By 2001, the AHCPR Cardiac Rehabilitation Guidelines stated that exercise training in patients with heart failure decreases symptoms, improves exercise tolerance, provides additive benefits to ACE inhibitor therapy, and doesn’t worsen left ventricular function. Dr. Andrew JS Coats, University of Sidney, reviewed the evidence on the effects of exercise training in patients with heart failure. Initial studies were restricted to physiological parameters such as maximal oxygen consumption or exercise time. A 1989 study showed that physical training improved ventilatory responses in patients with CHF. In 1990 and 1992, Dr. Coats, et al published results of a randomized trial of exercise training in patients with stable, Class II/III CHF. After eight weeks of home-based cycle training, patients had a 25% increase in peak VO2, and improved symptoms, neurohormonal balance, and exercise capacity.
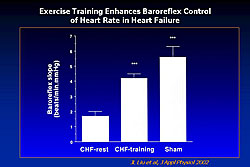
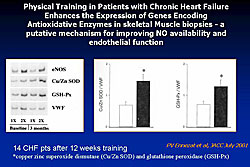
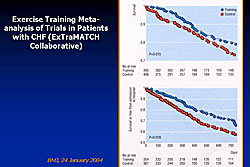
The Leipzig Heart Failure Training Trial demonstrated significantly increased peak exercise, reduced LV end-diastolic diameter, and increased stroke volume at rest and at peak exercise in CHF patients randomized to exercise training. In the ELVD-CHF Trial, antiremodeling effects were observed in CHF patients after six months of exercise training, with reduced end-diastolic volume (EDV) and end-systolic volume (ESV) and increased ejection fraction (EF). Randomized trials have demonstrated that exercise training improves skeletal muscle metabolism, mitochondrial oxidative capacity, peak work rate, strength and endurance. Beneficial effects have also been observed in parameters proven to be adverse prognostic markers in heart failure. Among the benefits demonstrated in randomized trials are attenuation of ergoreflex hyperactivation, improvement of autonomic dysfunction, and enhanced baroreflex control of heart rate (Figure 1). Physical training corrects endothelial dysfunction. A study showing that exercise enhances the expression of genes encoding antioxidative enzymes in skeletal muscle proposed this as a mechanism for improved nitric oxide (NO) availability and endothelial function with exercise (Figure 2). Exercise training in CHF patients also has anti-inflammatory effects, significantly reducing TNF-α levels from baseline (P<0.01). A correlation has been observed between training-induced changes in adhesion molecules and improvements in exercise tolerance. A recent meta-analysis of exercise training trials in patients with CHF (ExTraMATCH Collaborative) found a significant improvement in survival (P=0.015) and a significant reduction in the combined endpoint of death or hospitalization for CHF (P=0.018) (Figure 3). The planned ACTION trial will prospectively investigate the effects of exercise training on all cause mortality and hospital admissions in patients with CHF. |
|
|
|
Copyright © 2007 Japanese Circulation Society All Rights Reserved. webmaster@j-circ.or.jp |