 |
|
|
 |
| Assessment of Coronary Artery
Disease by Contrast Echocardiography |
|
|
Fuminobu Ishikura, M.D.
Osaka University,
Osaka, Japan
Takashi Muro, M.D.
Osaka City University,
Osaka, Japan
Young-Jae Lim, M.D.
Department of Cardiology,
Kawachi General Hospital
Sanjiv Kaul, M.D.
University of Virginia,
USA
|
|
|
|
 |
|
|
 |
|
Myocardial
Contrast Echocardiography |
|
Experts who spoke at this panel discussion agreed
that myocardial contrast echocardiography (MCE) is
a promising technique for assessment of myocardial
viability because it provides direct visual assessment
of regional myocardial perfusion. “MCE is the
most powerful method of assessing myocardial perfusion
and should be used at the first sign of ischemia,”
said Fuminobu Ishikura, MD, of Osaka University.
MCE provides the real-time information about
which areas of the myocardium are ischemic that is
not gained with intermittent myocardial imaging, which
is currently used in Japan. The advantages of real-time
imaging with MCE are the more precise identification
of the areas of ischemia and the information about
wall motion and myocardial perfusion that is simultaneously
provided. At present, real-time MCE is used in the
US, mainly in the research setting. This method should
be available in Japan in the near future.
“Real-time imaging can provide images of the
opacified myocardium in multiple cross sections. Stress
MCE will be a useful method to assess a myocardial
infarction and to detect the area jeopardized by coronary
stenosis,” stated Ishikura.
|
PAGE
TOP
|
Continuous
Intravenous Infusion of Contrast Agents |
|
Studies of continuous intravenous infusion using
Levovist, the only contrast media agent available
in Japan, to assess myocardial perfusion was presented
by Takashi Muro, MD, of Osaka City University. Muro
noted that this is a rather weak contrast agent, making
imaging studies a challenge.
Intravenous MCE has the potential for predicting
myocardial viability in both the acute and subacute
phases of myocardial infarction, said Muro. MCE assessment
of myocardial viability depends on an intact microcirculation.
Myocyte loss occurring as a result of myocardial infarction
results in a loss of microvasculature, according to
various studies. Therefore, the absence of myocardial
opacification on MCE may reflect a lack of myocardial
viability.
A study in 10 healthy volunteers demonstrated the
feasibility of the technique. “A quantitative
assessment of myocardial perfusion can be performed
with intravenous MCE, particularly using harmonic
power Doppler imaging with a continuous infusion of
Levovist,” Muro said.
Another study assessed myocardial perfusion in 15
patients with myocardial infarction using intravenous
MCE and compared it to positron emission tomography
(PET) in the same patients. PET is considered the
“gold standard” for myocardial imaging in
Japan. All the study patients had anteroseptal myocardial
infarction, indicating their lesions were well opacified
in four chambers.
|
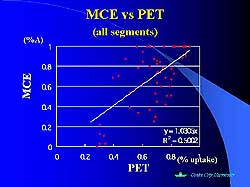 |
| Figure
1. The concordance between MCE and PET images
in all the study segments. |
| Click
to enlarge |
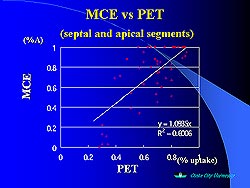 |
| Figure
2. The concordance between MCE and PET images
in all the septal and apical segments. |
| Click
to enlarge |
|
The concordance between MCE and PET was good in normal
and severely reduced segments of the myocardium, but
discordance between these two imaging modalities was
observed in the mildly reduced segments (Figure 1).
Many of the segments that were mildly reduced on PET
imaging appeared normal on MCE, suggesting that MCE
is not as sensitive as PET to mild perfusion abnormalities
(Figure 2).
“The concordance between MCE and PET is not
ideal, particularly when the focus is on the segments
around the left ventricle. Although intravenous MCE
has several limitations for identifying myocardial
viability, this non-invasive technique should be a
useful tool for clinical practice,” stated Muro.
|
PAGE
TOP
|
MCE to Assess
Collateral Function |
|
The value of MCE in assessing collateral vessel function
compared to coronary angiography (CA) was studied
by Lim and colleagues. Visualization of epicardial
coronary collateral vessels by CA does not provide
functional information about these vessels, because
the presence of collaterals does not necessarily mean
that myocardial perfusion is occurring, explained
Young-Jae Lim, MD, Department of Cardiology, Kawachi
General Hospital. CA visualizes vessels > 100 microns
and demonstrates epicardial arterial conduits. MCE
uses microbubbles that can traverse smaller collateral
networks, can visualize myocardial tissue perfusion,
and delineates the occluded bed area and pre-perfusion
residual flow.
MCE is an alternative method to CA for the assessment
of dynamic collateral circulation at rest and during
stress. Intravenous MCE would be a unique noninvasive
method of assessing coronary collateral function,
if studies show that intravenous and intracoronary
MCE are equally valuable methods of assessing collateral
function. However, several problems remain to be overcome
before intravenous MCE can be applied in the clinical
setting, including the need for real-time imaging
instead of intermittent imaging, the limited angular
view possible at present, and the need for improved
clarity of myocardial staining.
|
PAGE
TOP
|
Capillaries
and Coronary Blood Flow Reserve |
|
For many years, it has been generally assumed that
resistance due to coronary stenosis prevents an increase
in hyperemic myocardial blood flow, which leads to
a reduction in coronary blood flow reserve. Kaul and
colleagues performed studies using contrast echocardiography,
which demonstrated that, in fact, an increase in capillary
resistance is the major reason for decreased coronary
flow reserve in the presence of a stenosis. “The
resistance offered by the stenosis itself plays only
a small role in reducing coronary flow reserve,”
stated Sanjiv Kaul, MD, University of Virginia, USA.
Contrast echocardiography allows visualization of
the capillary circulation. The capillaries are the
“bottleneck” for hyperemic flow during maximal
hyperemia in normal people. Any condition, including
hyperlipidemia and hyperglycemia, that changes capillary
resistance and blood viscosity will change hyperemic
flow.
The greater the number of capillaries present, the
less resistance and the higher the hyperemic coronary
blood flow. If the capillary number is reduced, as
in diabetes, hypertension, or myocardial infarction,
coronary blood flow is reduced even in the absence
of a stenosis. In the presence of a stenosis, there
is de-recruitment of capillaries distal to the stenosis
during hyperemia, resulting in increased capillary
resistance.
Even in the presence of stenosis, capillaries remain
the major determinant of reduction in hyperemic flow
because of de-recruitment of capillaries distal to
the stenosis. This in turn causes perfusion defects.
This may be the reason that hyperlipidemia plus stenosis
may be much worse than hyperlipidemia in the absence
of stenosis or vice-versa. It appears that more than
one factor can cause an increase in capillary resistance,
a decrease in capillary blood volume and a change
in blood viscosity.
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2001
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|