 |
|
|
 |
| Medical and Surgical Treatments
for End-Stage Heart Failure |
|
Yukihiro Koretsune, M.D.
Osaka National Hospital,
Osaka, Japan
Satoshi Ubutaka, M.D.
Jichi Medical School,
Tochigi,
Japan
Akira Kawaguchi, M.D.
Tokai University,
Isehara, Japan
Takeshi Nakatani, M.D.
National Cardiovascular
Center, Osaka, Japan |
|
|
|
 |
|
|
 |
|
The effects of intermittent
milrinone therapy on mortality and cardioprotection
have not been clarified, although it has been shown
to improve quality of life and allows for hospital discharge
of severe chronic heart failure patients. The effects
of milrinone infusion on cardiac function, hemodynamics,
autonomic nerve activity in patients with chronic heart
failure was reviewed by Yukihiro Koretsune, MD, Osaka
National Hospital.
In this study, a 4-hour infusion of milrinone (0.5 mcg/kg/min)
was given to 10 patients (mean age 66 years, 5 female,
1 NYHA class II, 7 NYHA class III) and a 6-hour infusion
to 6 patients (mean age 63 years, 2 female, 1 NYHA class
II, 4 NYHA class II, 1 NYHA class IV) for one week.
No significant changes in blood pressure, left ventricular
(LV) systolic function, LV dimension or total bilirubin
was seen in either group over the study period. A significant
reduction in heart rate (from 77 to 71 beats per minute)
was observed 3 days after initiation of the 4-hr infusion.
A sustained decrease in BNP was observed for 3 days
after the 4-hr infusion in the five patients with 500
pg/ml or more of BNP at baseline. The decrease in BNP
returned to the baseline values 6 days after infusion.
The decrease in BNP was not observed with the 6-hr infusion.
These results suggest that a 4-hr infusion of milrinone
for three days may obtain a sustained decrease in heart
rate and BNP.
Results from a study of 8 patients (mean age 67 ears,
2 female) who received intermittent milrinone therapy
(4-hr infusion twice per week) suggest this therapy
may be cardioprotective, as indicated by the increase
in CVR-R, an indicator of parasympathetic nerve activity.
Further, there was a progressive decrease in BNP in
the patients with a baseline BNP greater than 300 pg/ml.
|
PAGE
TOP
|
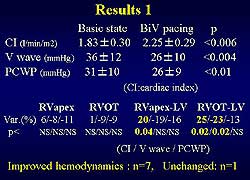 |
| Figure
1. Results in acute study of 8 patients. (Ubutaka
S, Ritter P) |
| Click
to enlarge |
|
Theoretically,
synchronous bi-ventricular pacing with the LV electrode
placed at the base of the heart could counteract the
reverse activation sequence induced by the right ventricular
(RV) pacing. The presence of fibrous tissue due to the
underlying diseases causes heterogeneity of the transmission
of the heart excitation. Three types of asynchronies
result from this heterogeneity, AV, intraventricular
and interventricular. The goal of pacing therapy is
to normalize these asynchronies.
In an acute study of 8 patients, bi-ventricular pacing
was associated with significant improvements from baseline
in cardiac index, V-wave and PCWP (Figure 1). No statistically
significant change was observed with RV pacing in RV
apex and RVOT. But with Bi-ventricular pacing, there
was a significant change in the RV apex-LV and RVOT-LV
leading to a change in the cardiac index. Bi-ventricular
pacing improved the hemodynamics in 7 patients, while
no change was seen in one patient, stated Satoshi Ubutaka,
MD, of Jichi Medical School. The mean age of the patients
was 66 years, male 7, LVEF 22%, NYHA class IV 8, and
QRS duration 200 ms (120-240 ms). |
 |
| Figure
2. Results in 50 patients receiving chronic bi-ventricular
pacing. (Ubutaka S, Ritter P) |
| Click
to enlarge |
|
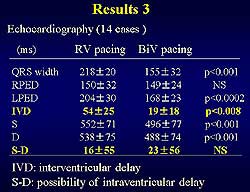
An evaluation
of bi-ventricular pacing as a supplemental treatment
for refractory heart failure was also performed by this
group. This long-term study (1994-1997) of 50 patients
who received chronic bi-ventricular pacing showed a
consistent decrease in NYHA class, implying an improvement
in quality of life (Figure 2). The average follow-up
was 13 months and the average NYHA class was 2.3. There
were 17 deaths (11 heart failure, 4 sudden cardiac death,
2 non-cardiac). Bi-ventricular pacing served as a bridge
to transplant for 3 patients. IVD shortening was seen
in the patients with bi-ventricular pacing compared
to RV pacing (19 vs 54 ms), showing a change in interventricular
delay. No significant change was seen in the intraventricular
delay. The mean age was 68 years, male 47, NYHA class
III 14, NYHA class IV 36 patients. |
PAGE
TOP
|
Partial Left
Ventriculectomy |
Data from an international
registry of patients who underwent partial left ventriculectomy
(PLV) was reviewed to provide insights regarding outcomes
and patient selection criteria. In brief, PLV was associated
with better survival in less symptomatic patients with
better contractile reserve undergoing elective surgery
preserving the papillary muscles. The recent improvement
in survival appears to be related to improved patient
selection by experienced hospitals (> 5 cases performed)
based on identified risk factors. While “high risk”
patients have an indication for transplantation, PLV
may be indicated for “low risk” patients without
back-up transplantation available and to reduce necessity
for transplantation (NYHA < class III, %FS < 12%
are criteria). Rescue transplantation may improve survival
after PLV, which may ease donor shortage by improving
graft availability. PLV and transplantation are complementary
approaches.
Survival rates did not differ between Asia, Europe and
the US, and no difference was seen between Japanese
and non-Japanese. Factors related to better survival
were patients with larger body size, male gender, NYHA
class < IV, fractional shortening > 12% compared
to FS < 5%, duration of heart failure < 3 years,
and < 4 hospitalizations for heart failure. The pre-operative
cardiac heart failure condition had a great effect on
survival. |
 |
| Figure
3. Survival by etiology of heart failure in patients
who underwent partial left ventriculectomy. |
| Click
to enlarge |
|
The underlying
disease was dilated cardiomyopathy (DCM) in 92%, valvular
4.2%, dilated hypertrophic cardiomyopathy (DHCM) 1.4%
and other in 2.4%. In terms of survival by etiology,
no significant difference was observed, although it
was somewhat lower in DCM and valvular disease than
in coronary artery disease (Figure 3). In the registry,
82% were male, and 28% > age 50years, 32% > age
60 years and 17% > 65 years. Survival was better
in those < 60 years,
Fewer than 1 in 4 patients who underwent emergency PLV
survived. Long-term prognosis was poor with an LV mass
> 400 g. An indication for transplantation was associated
with better survival compared to no indication. Survival
was better in institutions that had performed more than
5 cases and even greater in those that had performed
more than 10 cases. A learning curve for performing
PLV is indicated by the improved survival after 1999.
In summary, patient risk factors are age> 65 years,
NYHA IV, % FS < 5%, emergency PLV, heart failure
duration > 9 yrs and no indication for transplantation.
|
PAGE
TOP
|
Left Ventricular
Assist and Heart Transplantation |
The outcomes with left ventricular
assist support and heart transplantation in patients
with end-stage heart failure at the National Cardiovascular
Center in Japan was reviewed by Takeshi Nakatani, MD.
Extracorporeal ventricular assist system (VAS) was used
in 35 patients (30 DCM, 1 DHCM, 4 ischemic CM, mean
age 34 years with range of 8-57 years, 25 male). LVAS
was used in 30 patients, 10 of whom received the left
atrial drainage type (LA-LVAS) while 20 received the
LV drainage type system (LV-LVAS). Biventricular support
(Bi-VAS; LVAS plus right VAS) was used in 5 patients.
|
 |
| Figure
4. The duration of LV-VAS support in the study
population. |
| Click
to enlarge |
|
Of the 35 patients
on VAS, 4 were weaned (3 discharge, 1 death), 16 died
on VAS (2 in < 30 days, 10 candidates for transplant),
7 received a transplant, and 8 continue VAS. The average
duration of assist was 224 days, with a range of 7-668
days (Figure 4). The major causes of death are infection,
cerebral embolism and bleeding.
Regarding heart transplantation, 5 of the 6 cases at
the National Cardiovascular Center had been on LVAS.
The number of days waiting for a transplant ranged from
29 to 628 days. Three of the 6 patients have returned
to work and 3 remain in hospital. The bicaval approach
was used in 5 and the Lower-Shumway in one. There have
been no serious complications or rejections to date.
Nakatani concluded that LVAS and heart transplant are
optimal options for end stage heart failure, and that
LV-LVAS especially is a good bridge to transplant. |
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2001
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|