 |
|
|
 |
| Blood Pressure Control for Prevention
of Renal Complications |
|
Atsuo Goto, M.D.
University of Tokyo,
Tokyo, Japan
Hiroo Kumagai, M.D.
Keio University, Tokyo,
Japan
Naofumi Ikeda, M.D.
Saitama Medical School,
Saitama, Japan
Edward D. Frohlich,
M.D.
Alton Ochsner Medical
Foundation, New Orleans, Louisiana |
|
|
|
 |
|
|
 |
|
End-stage renal disease
is increasing in the US and Japan. This is primarily
related to patients who have hypertension and diabetes.
Diabetologists have rightly shown that diabetes is most
important and therefore deserves increased attention,
stated Edward D. Frohlich, MD, Alton Ochsner Medical
Foundation in New Orleans.
The lack of adequate hypertension control is considered
by some to be the reason that the target organ involvement
of the kidney has not been as responsive as that in
stroke and CHD. However, others state that the renal
involvement might not be reversible with antihypertensive
treatment, or that the antihypertensive agents used
in the past were not effective against renal problems.
Intrarenal hemodynamic effects of hypertensive vascular
disease include ischemia of the kidney, hyperfiltration
at the glomerular level associated with protein deposition
and glomerulosclerosis, and arteriolar hyalinosis. |
|
Progression
of Renal Function: Effect of Blood Pressure Control
|
Systolic blood pressure
control and proteinuria determined the rate of decline
in renal function in renal parenchymal disease (RPD),
concluded Dr. Goto of the University of Tokyo, based
on their retrospective, longitudinal study. Further,
although renal function is usually stable in essential
hypertension (EH), the prevention of renal dysfunction
may require close attention to proteinuria, age and
blood pressure.
Goto and colleagues analyzed the data of 389 EH patients
and 106 RPD patients who visited their clinic from 1991-1998
who were followed for a minimum of 3 years, with >
3 blood pressure measurements and > 3 serum creatinine
measurements at 6-month intervals. Significant differences
in baseline characteristics were older age in the EH
compared to the RPD group (58 vs 49 years, p<0.001)
and higher serum creatinine in the RPD vs EH group (1.65
vs 0.95; p<0.001). At follow-up, there was higher
serum creatinine in the EH vs RPD group (7.6 vs 5.7
mg/dl, p<0.001). The pre-treatment blood pressures
were 169/103 in the EH group and 157/97 in the RPD group
(p<0.01). Fifty-six percent of the EH group and 49%
of the RPD group achieved a blood pressure < 140/90,
which required at least two agents in each group. |
 |
| Figure
1. In the patients with renal parenchymal disease,
the rate of decline in renal function was faster
than in the patients with essential hypertension.
|
| Click
to enlarge |
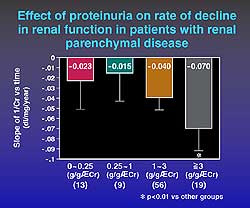 |
| Figure
2. Renal function progresses in relation to the
increase in proteinuria. |
| Click
to enlarge |
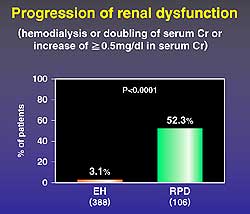 |
| Figure
3. The rate of renal dysfunction in the patients
with essential hypertension and renal parenchymal
disease. |
| Click
to enlarge |
|
Renal function
declined faster in the RPD group compared to the EH
group (p<0.001) (Figure 1). In the RPD group, better
blood pressure control was related to slower progression
of renal dysfunction, as shown by dividing the patients
based on SH (>140) versus SN (<140). The slope
of the reciprocal of serum creatinine (Cr) vs time (dl/mg/yr)
in the SH group was –0.056 and in the SN group
–0.031, p<0.01). There was no difference in
proteinuria, antihypertensive agent used or pre-treatment
blood pressure. No significant difference in relation
to ACE inhibitor use was observed.
In RPD, the higher the level of proteinuria, the faster
the progression of renal dysfunction (Figure 2). The
determinants of decline in EH were proteinuria (-0.278)
and age (-0.157), and in RPD they were proteinuria (-0.255)
and systolic blood pressure (-0.294).
Renal dysfunction (hemodialysis, doubling of serum creatinine,
increase > 0.5 mg/dl in serum Cr) progressed in 3.1%
of the EH group and 52.3% of the RPD group (p<0.001)
(Figure 3). A relation between higher proteinuria and
worse blood pressure control was seen in the RPD group.
The predictors of disease progression in the EH group
were SBP, DBP, and initial creatinine (all p<0.01
vs patients without progression). |
PAGE
TOP
|
ARB in Moderate
Renal Dysfunction |
| Proteinuria was reduced
more with an angiotensin receptor blocker (ARB) than
with an ACE inhibitor in a randomized, prospective 1-year
study that sought to compare the effects of these two
drugs on proteinuria and renal function in hypertensive
patients with moderate renal dysfunction. Blood pressure
reduction and other factors were shown to be important
in the reduction of proteinuria and maintenance of renal
function. The “escape” phenomenon of aldosterone
(re-elevation of plasma aldosterone concentration) was
not found in the ARB group. In the ACE I group some
evidence of this escape phenomenon was seen. The magnitude
of reduction in proteinuria was positively correlated
with the decrease of aldosterone level. A blood pressure
of less than < 130/85 appears to be an appropriate
goal for renoprotection, stated Hiroo Kumagai, MD, of
Keio University in Tokyo. |
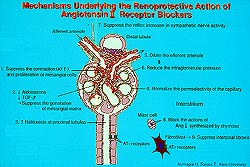 |
| Figure
4. The mechanisms involved with the renoprotective
ability of angiotensin receptor blockers. |
| Click
to enlarge |
|
In terms of
the renoprotective mechanism, ARBs and ACE inhibitors
dilate the efferent arterioles and reduce the intraglomerular
pressure. ARBs block the action of angiotensin II synthesized
by chymase in the interstitium, and suppress interstitial
fibrosis. ARBs better suppresses aldosterone production,
which has been shown to upregulate the TGF-beta and
contributes to the generation of the mesangial matrix.
It may be that the ARBs suppress the generation of the
mesangial matrix (Figure 4).
In this study, 49 patients with hypertension with renal
impairment (serum Cr 1.3-3.0 mg/dl and/or proteinuria
>70 mg/dl) due to chronic glomerulonephritis, diabetes
or essential hypertension were randomized to candesartan
(4-8 mg/day) or losartan (50-100 mg/day) or ACE inhibitor
(n=25). Seventy-five percent of all patients required
the addition of a calcium antagonist to achieve the
blood pressure goal < 130/85.
Proteinuria was better reduced with the ARB (214 to
61 mg/dl, p<0.01) than with the ACE I (202 to 93
mg/dl, p<0.05). A renoprotective effect of the ARB
was suggested by stable serum Cr during the study (2.0
± 0.4 to 2.2 ± 0.5 mg/dl). The serum Cr
level was similar for the ACE inhibitor. There was a
transient 20% increase in serum Cr during the first
1-3 months, which was decreased by about 1 month and
was maintained.
Serum potassium was significantly increased at 6 months
and maintained with both the ARB (from 4.4 to 5.3 mEq/l)
and the ACE I (from 4.3 to 5.2 mEq/l; p<0.05 for
both), indicating the need for close observation by
the physician, stated Kumagai. Plasma aldosterone was
significantly reduced in correlation with the proteinuria.
The escape phenomenon was not seen in the ARB patients,
but seen in 4 of the 15 ACE inhibitor patients. |
PAGE
TOP
|
Congestive
Heart failure and Renal Insufficiency |
The appropriate degree of
blood pressure reduction in patients with heart failure
and chronic renal insufficiency (CRI) is uncertain.
Patients with heart failure, hypotension, hyponatremia
and volume depletion are more likely to experience a
substantial increase in the BUN level after treatment
with an ACE inhibitor. Thus, it may be that ACE inhibitor
treatment could aggravate renal dysfunction in patients
with heart failure. In the CONSENSUS heart failure trial,
serum Cr increased more than 2-fold in 11% of patients
and increased 30-100% in 24% of patients. In the SOLVD
trial, serum Cr was increased more than 2.0 mg/dl in
11% of patients.
A 2-year study to determine whether more intensive blood
pressure lowering was beneficial in heart failure patients
with CRI showed that tight blood pressure control <
120/75 (compared to usual blood pressure <130/80)
with a relatively small dose of an ACE inhibitor and
a long-acting calcium antagonist seemed to provide cardio-renal
protection in hypertensive patients with impaired cardiac
function and CRI. Although a lower level of blood pressure
may be effective for organ protection, stated Naofumi
Ikeda, MD, Saitama Medical School, it is unknown whether
these results can be extrapolated to patients with other
types of heart disease. |
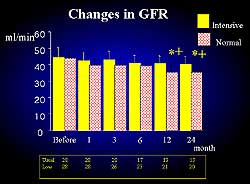 |
| Figure
5. Improvements in the glomerular filtration rate
was related to improvements in survival. |
| Click
to enlarge |
|
In the 56 patients
studied (35 male, EF < 55%), at 2 years systolic
blood pressure was reduced from 150 to 118 in the intensive
group and to 128 in the usual group. At 2 years the
diastolic blood pressure was 73 in the intensive group
and 81 in the usual group. In terms of glomerular filtration
rate (GFR), no between group difference was seen until
6 months. At 1 year and 2 years the change in GFR was
greater in the usual group. Figure 5 shows the effect
of the change in GFR on survival. Survival at 24 months
was improved in the intensive group compared to the
usual group (Figure 6). The EF improved to about 60%
in the intensive group from 6 months to 24 months (Figure
7). |
|
|
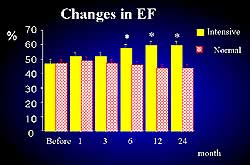 |
| Figure
7. Changes in the ejection fraction in the present
study. |
| Click
to enlarge |
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2001
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|