 |
|
|
 |
| Prevention and Treatment of Diabetic Cardiovascular Diseases: Progress at
the Turn of the Century |
|
Thomas K. Nordt
University of Freiburg, Freiburg,
Germany
Satoshi Fujii
Hokkaido University Graduate
School of Medicine, Sapporo, Japan
Shunichi Miyazaki
National Cardiovascular
Center, Suita, Japan
Ikuyoshi Watanabe
Nihon University Surugadai
Hospital, Tokyo, Japan |
|
|
|
 |
|
|
 |
|
Proven and
Promising Aspects of Prevention and Treatment |
|
In patients with diabetes mellitus, coronary artery
disease (CAD) is not only more common than in non-diabetic
persons (40% versus 2-4%) but is also more deadly.
Its presence not only increases the risk for cardiovascular
events, but worsens the prognosis in patients after
a myocardial infarction (MI) or revascularization
procedures. Mortality is increased two-fold in males
and four-fold in females when diabetes and CAD co-exist,
said Thomas K. Nordt, MD, of the University of Freiburg,
Germany, in his keynote lecture during this symposium.
Pathophysiologically, CAD in the setting of diabetes
is characterized by endothelial dysfunction, increased
platelet activity, increased coagulant activity, and
reduced fibrinolytic activity. This enhanced hemostatic
activity increases the frequency and severity of atherosclerotic
lesions and leads to the development of more microthrombi
that support the atherosclerotic lesion. Angiographically,
diabetic patients with CAD exhibit more diffuse and
more distally located lesions than their non-diabetic
counterparts and are more likely to have multivessel
and left main disease. This makes revascularization
procedures more challenging.
Diabetes is now considered a "CAD risk-equivalent,"
meaning that it contributes as much to the coronary
event risk profile as does a previous history of a
coronary event. The management of risk factors, therefore,
becomes the most important means of preventing CAD
in the setting of diabetes. The control of the underlying
diabetes is quite protective in this regard. The United
Kingdom Prospective Diabetes Study (UKPDS) of 3,867
type 2 diabetic patients demonstrated the value of
glucose control. Intensive glucose control with insulin
or sulfonylureas reduced the incidence of MI over
15 years as compared with conventional therapy. Every
1% increase in hemoglobin A1c (uncontrolled glucose)
was accompanied by a 40% increase in MI, but reductions
in hemoglobin A1c protected against fatal and non-fatal
MI as well as the microvascular endpoints of retinopathy,
nephropathy, and neuropathy. A similar association
is seen in type 1 diabetes. A clear correlation between
intensive insulin therapy or better glucose control
and delay of the onset of cardiovascular or microvascular
disease was shown in the Diabetes Control and Complications
Trial of 1,441 patients.
As for any person at risk for CAD, another important
risk factor is hypercholesterolemia. Target LDL levels
for diabetic patients are as strict as for patients
with existing CAD, and statins are an essential part
of the treatment plan. Statins have been shown to
not only reduce hypercholesterolemia but, in some
studies, to also protect against the development of
diabetes.
Platelet inhibition, beyond that achieved with aspirin,
is also important in the prevention of coronary events
in diabetics. In the CURE study [Clopidogrel in Unstable
Angina to Prevent Recurrent Events], patients with
acute coronary syndromes without ST segment elevations
(including diabetics) had a reduction in cardiovascular
deaths, MI, and stroke when they received clopidogrel
in addition to aspirin, versus aspirin alone. Other
studies have substantiated the benefit of the glycoprotein
IIb/IIIa inhibitors in acute coronary syndromes. In
diabetics, pooled analysis of the major trials showed
30-day mortality to be 4.6% with these agents versus
6.2% without (Circulation 2001;104:2767-71). Their
obvious benefit in diabetics may be based on the fact
that diabetics have highly activated platelets as
well as GPIIb/IIIa receptors. The meta-analysis, however,
did not include GUSTO V, which found no benefit of
adding the GPIIb/IIIa inhibitor abciximab to reteplase,
a tissue plasminogen activator (Lancet 2001;357:1905-14),
either in the whole population or in diabetics.
Finally, with regard to interventional therapies,
it appears that angioplasty may produce a worse outcome
than coronary artery bypass grafting. This was suggested
by the results of the Bypass Angioplasty Revascularization
Investigation (BARI) of 22 patients with multivessel
disease. In nondiabetic patients, all-cause and cardiac
mortality was similar between the arms, but diabetic
patients had a worse outcome after angioplasty. This
was also shown in the Arterial Revascularization Therapy
Study among diabetic patients who received angioplasty
with stenting, versus bypass grafting.
|
PAGE
TOP
|
Diminished
Left Ventricular Function, Coronary Perivascular Fibrosis
and Increased Plasminogen Activator Inhibitor-1 Expression
Associated with Insulin-Resistant Mice |
|
Plasminogen-activator inhibitor-1 (PAI-1) may be
a novel therapeutic target for cardiovascular diseases,
according to research presented by Satoshi Fujii,
of the Hokkaido University Graduate School of Medicine,
Sapporo. These investigators previously showed that
coronary perimicrovascular fibrosis is augmented by
increased cardiac expression of PAI-1, an inhibitor
of proteolysis (fibrinolysis) in genetically obese
mice with insulin resistance. The present study was
performed to explore the potential role of insulin
receptor substrate-1 (IRS-1)-mediated signaling in
heart PAI-1 expression in wild type (C57BL/6J) and
IRS-1 knock-out (KO) mice.
PAI-1 is the primary physiological inhibitor of fibrinolysis.
Hypofibrinolysis can induce intravascular thrombosis
by decreasing fibrin degradation, migration of vascular
smooth muscle cells and accumulation of extracellular
matrix. In subjects with insulin resistance, increased
PAI-1 levels may reflect insulin-dependent and pro-insulin-dependent
augmentation of the synthesis of PAI-1 by hepatic,
vascular and adipose cells, but in heart tissues,
PAI-1 expression and its influences and mechanisms
are not fully understood.
|
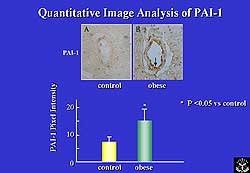 |
| Figure
1. Myofiber diameters were reduced in the knock-out
mice on quantitative image analysis of PAI-1 in
tissue samples. |
| Click
to enlarge |
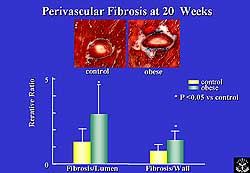 |
| Figure
2. Perivascular fibrosis-to-lumen ratio and wall-to-lumen
ratio was significantly increased in the IRS-1
KO mice compared to controls. |
| Click
to enlarge |
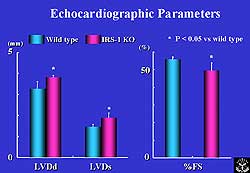 |
| Figure
3. Diastolic and systolic LV diameters were significantly
increased and fractional shortening was decreased
in IRS-1 KO mice compared to controls. |
| Click
to enlarge |
|
In the experimental
animals, at 20 weeks of age, the ratio of left ventricular
(LV) weight to body weight was increased in the KO mice
compared to controls, suggesting the presence of LV
hypertrophy. Quantitative image analysis of PAI-1 in
tissue samples showed myofiber diameters to be reduced
in the KO mice (by lower pixel intensity), suggesting
that IRS-1-mediated signaling may be important for normal
cardiac growth and development (Figure 1); in addition,
along with myocyte atrophy, the IRS-1 KO mice exhibited
significantly increased perivascular fibrosis-to-lumen
ratio and wall-to-lumen ratio versus controls,(Figure
2) suggesting the coronary arteries may undergo substantial
remodeling in spite of the lack of IRS-1 signaling.
Interestingly, the perivascular fibrosis was accompanied
by high PAI-1 mRNA expression in the heart, suggesting
that IRS-1-mediated signaling may not be so important
in PAI-1 expression in cardiac tissues.
Cardiac function was evaluated by 15 MHz high-resolution
echocardiography. In these studies, diastolic and
systolic LV diameters were found to be significantly
increased in IRS-1 KO mice and fractional shortening
was decreased, indicating dilatation and dysfunction
in the KO animals (Figure 3). Without IRS-1-mediated
signaling, cardiac function may be diminished, the
results suggested.
In sum, perimicrovascular fibrosis was augmented
in genetically obese mice characterized by insulin
resistance, hyperglycemia, hyperinsulinemia, and non-insulin-dependent
diabetes. LV dysfunction, coronary perimicrovascular
fibrosis, and increased cardiac PAI-1 expression associated
with insulin resistance still occurred, despite the
lack of IRS-1. It seems, therefore, that in the setting
of insulin resistance, PAI-1 expression is not fully
controlled by IRS-1-mediated signaling. PAI-1 may
be an attractive therapeutic target for the prevention
and treatment of diabetic vascular diseases, Dr. Fujii
stated.
|
PAGE
TOP
|
Abnormal
Glucose Tolerance and Long-Term Prognosis After Coronary
Angioplasty |
|
In diabetic patients undergoing coronary angioplasty,
good glycemic control may improve long-term survival,
according to a study from the National Cardiovascular
Center, Suita, Japan, which showed that abnormal glucose
tolerance was a greater predictor of prognosis than
small vessel diameter. The interventional outcomes
of patients with diabetes are known to be poorer than
for non-diabetic persons, and the question has been
whether this is due to diffuse disease that results
in a small final lumen or to the diabetes itself.
|
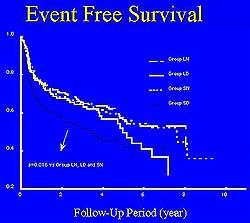 |
| Figure
5. Five-year event-free survival in the study
population. |
| Click
to enlarge |
 |
| Figure
6. Variables studied in relation to cardiac events
and mortality. |
| Click
to enlarge |
|
The study, reported by Shunichi Miyazaki, included
559 patients who underwent their first successful
elective balloon angioplasty (without stenting) between
1985 and 1990. Of these, 69 had diabetes and 120 had
impaired glucose tolerance, comprising the "abnormal
glucose tolerance" (AGT) subset. All patients were
divided into four groups according to the presence
of AGT and their final vessel diameter. Patients without
AGT and < 2.5 mm diameter were considered the "small-normal"
group; those without AGT and > 2.5 mm were the
"large-normal" group; those with AGT and < 2.5
mm were the small-DM (diabetes mellitus) group; and
those with AGT and > 2.5 mm were the "large- DM"
group. The endpoints were death, cardiac death, and
cardiac events, including non-fatal MI, repeat revascularization,
or death. The baseline characteristics of the study
population are shown in Figure 4.
Survival analysis at 5 years showed a worse event-free
survival for patients with AGT, especially the small-DM
group (Figure 5). The small-normal patients (who had
normal glucose tolerance and small vessel diameter)
had a similar event-free survival curve as the large-
DM and large-normal groups.
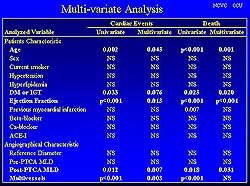
In a multivariate analysis, the cardiac events were
associated with the presence or absence of AGT (Figure
6). Among the four groups, event-free survival was
poorest for the small-DM patients; event-free survival
in the small-normal was similar to the large-DM and
large-normal patients up to 5 years, though for the
large-DM patients survival declined suddenly and inexplicably
5 years after intervention. Importantly, final vessel
diameter was not predictive of long-term survival,
while on the contrary the presence of AGT was an important
determinant, Dr. Miyazaki reported.
The patients were further evaluated for their level
of glycemic control, with hemoglobin A1c levels <
6.0 considered poor control and those > 6.0 representing
good control. Poorly controlled AGT patients had the
worse event-free survival, while AGT patients who
were well controlled had survival similar to non-diabetic
patients. The investigators concluded, therefore,
that good control of blood sugar levels is an important
means of improving outcomes in diabetic patients undergoing
angioplasty.
|
PAGE
TOP
|
Treating
Insulin Resistance in Non-Diabetic Patients |
|
Non-diabetic patients with insulin resistance should
be treated to prevent the development of coronary
artery disease (CAD), according to the results of
a study from Nihon University Surugadai Hospital,
Tokyo.
Ikuyoshi Watanabe, who presented the study, pointed
out that the relationship between insulin resistance
and CAD receives attention, but insulin resistance
is also associated with arteriosclerotic diseases
such as ischemic heart disease. The study investigated
the relationship between insulin resistance and endothelial
vasomotor function of the coronary artery of non-diabetic
patients with chest pain, to elucidate the significance
of insulin resistance in CAD.
|
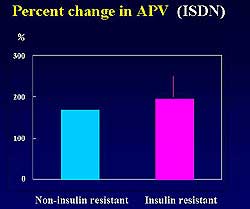 |
| Figure
8. No significant difference was seen in the percent
change in average peak flow velocities in the
insulin resistant (IR) and non-insulin resistant
(NIR) groups after administration of papaverin
and isosorbide dinitrate. |
| Click
to enlarge |
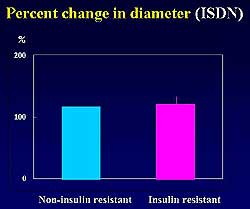 |
| Figure
9. Papaverin and isosorbide dinitrate administration
caused little difference in the percent changes
in diameter in the IR and NIR groups. |
| Click
to enlarge |
|
The study included 25 non-diabetic patients with
chest symptoms, who were divided into an insulin resistant
(IR) group (plasma glucose level >/= 135 mg/dL)
and a non-insulin resistant group (NIR) (< 135
mg/dL). The patient characteristics are shown in Figure
7. The effect of acetylcholine, papaverin, and isosorbide
dinitrate on the vasomotor response of the coronary
endothelium was studied and compared between the groups.
The percent change in diameter of the coronary artery
after injection of acetylcholine (20 microgram/ml/min)
was 84 +/- 17% in the IR group and 109 +/- 18% in
the NIR group (p < 0.01). The percent change in
coronary flow velocity after injection of acetylcholine
(20 microgram/ml/min) was 120 +/- 67% in the IR group
compared to 256 +/- 58% in the NIR group (p < 0.01).
The increase in coronary artery flow velocity in the
IR group was significantly smaller than that of the
NIR group (p < 0.01).
Papaverin and isosorbide dinitrate were injected
to confirm coronary flow results without the influence
of the endothelial function. After the administration
of these control substances, the percent change in
average peak flow velocities in the IR and NIR groups
did not significantly differ between each other, nor
did the percent changes in diameter (Figures 8 and
9). The conclusion of the study was that non-diabetic
patients with insulin resistance have endothelial
vasomotor dysfunction, thus suggesting the possibility
that such patients may benefit from treatment to prevent
coronary heart disease.
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2002
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|