 |
|
|
 |
| Mechanism,
Treatment and Prevention of Hypertensive Cardiovascular Disease: Progress
and Remaining Problems |
|
|
|
 |
|
Role of Rho-Kinase in the
Pathogenesis of Hypertension: Therapeutic Potential of Rho- Kinase Inhibitors
in Hypertension
Yoshitaka Hirookaa
Kyushu University Graduate School
of Medical Sciences, Fukuoka, Japan
|
|
The Rho-kinase pathway appears to be involved in
the pathogenesis of hypertension, and Rho-kinase inhibitors
such as fasudil may have potential as antihypertensive
agents, according to studies from this group of investigators.
The Rho-kinase pathway is involved in various functions,
including calcium sensitization and contraction of
vascular smooth muscle cells. Several key findings
from these investigators point to a role for Rho-kinase
in hypertension. First, in the spontaneously hypertensive
rat model, upregulation of Rho-kinase in blood vessels
was associated with vascular hyper-reactivity and
this preceded the development of hypertension. In
spontaneously hypertensive rats (SHR) as well as angiotensin
II-induced hypertensive rats, Rho-kinase was substantially
involved in vascular lesion formation, and the Rho-specific
inhibitor fasudil inhibited vascular lesion formation.
|
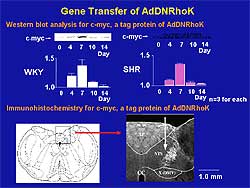 |
| Figure
1. Gene transfer study to confirm the
effect of Rho-kinase inhibitors. Western blot analysis and immunohistochemistry
for c-myc, a tag protein for DNRRhoK, confirmed the successful gene transfer.
Left panel shows time course of c-myc expression. Right panel quantifies the
time course. |
| Click
to enlarge |
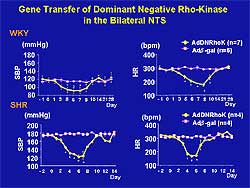 |
| Figure
2. The significant decrease in systolic blood pressure and heart
rate over 5-7 days was greater in the SHR than the WKY rats. The time course
of changes in blood pressure and heart rate correspond to the time course
of c-myc expression. |
| Click
to enlarge |
|
Secondly, activation of the Rho-kinase pathway occurs
within the central nervous system and is associated
with hypertension. SHR showed increased membrane expression
of Rho-A
and activity of Rho-kinase in the brainstem, and blockade
of Rho-kinase expression with Rho-kinase inhibitors
(Y-27632 or fasudil) produced a decrease in blood
pressure and sympathetic nerve activity. Normal Wistar-Kyoto
rats demonstrated less expression and less effect
on blood pressure with Rho-kinase inhibitors. Similar
findings were also demonstrated in an experiment using
adenovirus vector encoding dominant-negative Rho-kinase
(Figures
1 and 2).
Finally, in controlled studies in humans, fasudil
increased forearm blood flow in patients with essential
hypertension, but not in normotensive subjects, and
it normalized angiotensin-II-induced forearm vasoconstriction
in normotensive subjects.
Altogether, these observations indicate that Rho-kinase
is substantially involved in the mechanism of hypertension
related to the activation of the renin-angiotensin
system and the sympathetic nervous system. These data
suggest there may be a therapeutic role for Rho-kinase
inhibitors, which appear to preferentially mediate
the hypertensive state.
|
PAGE
TOP
|
Morning
Blood Pressure Surge and Associated Risk Factors for
Cardiovascular Disease in Hypertension
Kazuomi Kario
Jichi Medical School, Tochigi,
Japan
|
|
A morning surge in blood pressure is associated
with several cardiovascular disease-related risk factors
and an increased likelihood of stroke. Previous studies
have shown that the peak incidence of cardiovascular
events is in the morning hours, a time at which there
are also increases in ambulatory blood pressure (BP)
levels and tissue-type plasminogen activator inhibitor-1
(PAI-1). These investigators evaluated the relationship
between these factors and cardiovascular risk in 519
hypertensive patients (mean age 72) without cardiovascular
disease at baseline. Patients underwent extensive
ambulatory BP studies, including assessment of morning
surge blood pressure (MS) and brain MRI to identify
silent cerebral infarcts.
Study subjects were classified as having MS (cut-off
of 55 mm Hg) or no MS. By MRI analysis, the MS group
had a higher prevalence and greater number of silent
cerebral infarcts at baseline. At a mean follow-up
of 41 months, stroke incidence was also higher in
the MS group, with a relative risk of 2.7 independent
of age and 24-hour systolic BP level. Morning onset
of stroke was almost twice as common in the MS group
as the non-MS group. Thus, in hypertensives, exaggerated
MS was associated with an independent risk for hypertensive
target organ damage and cardiovascular events, Kario
reported.
As a possible source for the MS, the rate of orthostatic
hypertension was greatly increased among MS subjects,
as was systolic and diastolic BP, in a study sample.
Subjects with orthostatic hypertension or hypotension,
compared with normotensives, also had a greater prevalence
of multiple lacuna infarcts. Exaggerated MS, therefore,
was associated with orthostatic hypertension, sympathetic
hyperactivity, and increased ambulatory BP variability.
Tests of platelet aggregation also showed significantly
higher spontaneous small-platelet-aggregates in the
morning in MS subjects, versus those without MS (103
vs 42 x 103 counts; p <0.0001), but no significant
differences in the evening. PAI-1 levels were not
higher in MS subjects than in non-MS subjects. Patients
with multiple silent infarcts also had higher levels
of small-size platelet aggregates, PAI-1, and indicators
of thrombin generation and endothelial stimulation.
“The exaggerated morning blood pressure surge
and morning hypertension could be a new therapeutic
target for more effective prevention of cardiovascular
events in hypertensive patients,” Kario stated.
|
PAGE
TOP
|
Candesartan
Can Reduce Cardiovascular Events By Decreasing Sympathetic
Nerve Activity and Plasma Aldosterone
Hiroo Kumagai
Keio University School of Medicine,
Tokyo, Japan
|
|
The angiotensin receptor blocker (ARB) candesartan
was shown to affect a number of factors that relate
to increased cardiovascular risk and target organ
damage from hypertension, in a series of studies presented
by Hiroo Kumagai and colleagues from Keio University
School of Medicine, Tokyo.
When neurons of the rostral ventrolateral medulla
oblongata (RVLM), the sympathetic center, of spontaneously
hypertensive rats were superfused with candesartan,
the ARB hyperpolarized the membrane potential of the
neurons and reduced the firing rates, outcomes that
did not occur in normotensive rats. Infusions of candesartan
also prevented an increase in renal sympathetic nerve
activity (SNA) when blood pressure was experimentally
decreased in SHR rats. In an additional experiment,
2 weeks administration of candesartan produced significant
suppression of renal SNA in the rats, versus vehicle,
despite significant increases in blood pressure and
renal blood flow. This experiment, along with previous
findings in humans, “strongly indicates that
candesartan can reduce peripheral SNA,” Kumagai
said.
Keio University researchers also found that candesartan
improved disorders of cardiovascular regulation. Normal
neurocardiovascular regulation (heart rate) is characterized
by low linearity and high non-linearity (ie, high
complexity) and is chaotic and dynamic, while abnormal
regulation of the cardiovascular system is characterized
by high linearity and low non-linearity (low complexity).
Patients with a reduced non-linear component of the
heart rate are at increased risk for cardiovascular
events, he said, as background.
In the current study, the cardiovascular system of
SHR was characterized by high linearity and low non-linearity,
and candesartan improved the linearity and therefore
the cardiovascular regulation.
Finally, the effect of candesartan on aldosterone
levels was evaluated in a 2-year prospective study
of 46 patients with glomerulonephritis. Both the ACE
inhibitor and candesartan reduced blood pressure similarly,
but the ARB produced greater reductions in proteinuria,
plasma aldosterone concentrations (Figure
1), and SNA. The reduction in aldosterone and
potentiated SNA should be protective against renal
interstitial fibrosis and other target organ damage,
therefore, candesartan may have renovascular and cardiovascular
protective actions, Dr. Kumagai said. Figure
2 shows the mechanisms by which ARBs are renoprotective.
|
|
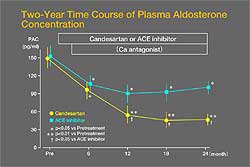 |
| Figure
1. Candesartan was associated with a greater reduction
in plasma aldosterone concentration (PAC) than
an ACE inhibitor in 46 patients with glomerulonephritis.
|
| Click
to enlarge |
|
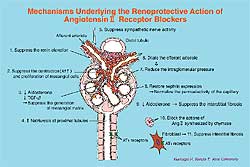 |
| Figure
2. Renoprotective mechanisms of angiotensin receptor
blockers. |
| Click
to enlarge |
|
PAGE
TOP
|
Hypertension
and Endothelial Function: Role of Angiotensin II and
Mechanical Pressure in Oxidative Stress
Yukihito Higashi
Graduate School of Biomedical
Sciences Hiroshima University, Hiroshima, Japan
|
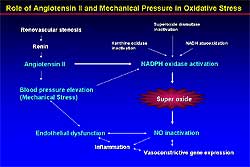 |
| Figure
1. Role of angiotensin II and mechanical pressure
in oxidative stress and endothelial dysfunction.
|
| Click
to enlarge |
|
Investigators from Hiroshima University examined
the mechanisms by which hypertension alters endothelial
function, and demonstrated the role of oxidative stress
induced by the activation of the renin-angiotensin
system.
As background, they noted recent reports that angiotensin
II stimulates the production of reactive oxygen species
through the activation of membrane-bound NADH/NADPH
oxidase (Figure
1). Endothelial dysfunction may be promoted when
an imbalance occurs: reduced production of nitric
oxide (NO) or increased production of reactive oxygen
species, mainly superoxide.
|
|
Patients with renovascular hypertension serve as
good models for determining how endothelium-dependent
vasodilation is affected by excess angiotensin II
and angiotensin II-related increases in oxidative
stress. Such patients have impaired endothelium-dependent
vasodilation induced by acetylcholine. In the study
presented by Higashi, this impairment (enhanced response
to acetylcholine) was restored by renal angioplasty
and by the infusion of the antioxidant vitamin C.
Furthermore, the improvement of endothelial function
correlated with the reduction in markers of oxidative
stress, such as 8-OHdG and MDA-LDL.
In addition, ACE inhibitors and angiotensin II receptor
blockers (ARBs) improved endothelial dysfunction of
forearm and renal circulation in patients with hypertension.
The effect was similar between the ACE inhibitor and
ARBs. Other antihypertensives (calcium antagonists,
beta blockers and diuretics) had no significant effect
on endothelial dysfunction, as judged by blood flow.
The improvement in endothelial function after angioplasty
or medication, however, did not correlate with a reduction
in blood pressure, the study also found.
These findings suggest that excess oxidative stress
generated by angiotensin II is involved, at least
in part, in impaired endothelium-dependent vasodilation
and that change in mechanical pressure generated by
high blood pressure may not directly promote the restoration
of endothelial function in human hypertension. ACE
inhibitors and ARBs augment endothelial function in
hypertensive patients, possibly due to NO production.
These agents should be able to improve endothelial
dysfunction and thus prevent cardiovascular complications,
Dr. Higashi said.
|
PAGE
TOP
Mechanism
of Transition from Hypertrophy to Heart Failure
Tohru Masuyama
Osaka University Graduate School
of Medicine, Suita, Japan
|
|
Long-standing hypertension leads to left ventricular
hypertrophy (LVH), which leads to diastolic dysfunction
and progresses to diastolic heart failure (DHF). The
paucity of data on DHF is largely due to the lack
of an animal model, but Tohru Masuyama and colleagues
at Osaka University Graduate School have developed
a model in which compensatory LVH develops early and
progresses to heart failure (HF) by 90 weeks of age.
In this model, left ventricular diastolic dysfunction
was related to structural changes, progressive myocardial
hypertrophy, and ultimately myocardial fibrosis.
“In our model, hypertension caused structural
abnormalities, such as LVH and myocardial fibrosis.
The development of these structural abnormalities
is considered to lead to diastolic failure and thus
to DHF,” Dr. Masuyama said. Interestingly, treatment
with an angiotensin receptor blocker (ARB) but not
a calcineurin inhibitor prevented myocardial fibrosis.
Additionally, blood pressure patterns in the DHF model
were normal in the compensatory LVH stage but altered
in the HF stage. Increases in left ventricular end
diastolic pressure were observed only in the advanced
stage. The effects of blood pressure lowering on myocardial
fibrosis were minimal.
While LVH has been considered an adaptive response
to pressure overload, experiments in this model did
not demonstrate a direct effect. The structural changes
were closely related, however, to neurohumoral activation;
thus, neurohumoral activation appears to aid in the
transition from compensatory LVH to HF, he said.
The maladaptive LVH appears to be induced independently
of mechanical stress and by the activation of growth
factors and agonists binding to G-protein-coupled
receptors. Induction of these is mediated by the shedding
of heparin-binding epidermal growth factor (HB-EGF)
and/or by the generation of reactive oxygen species.
Alteration in Ca2+ handling in the hypertrophied myocyte
is also likely involved in the development of LVH
itself as well as in the myocyte relaxation abnormality.
The new inhibitor of HB-EGF shedding, KBR 7785, blocks
the shedding of HB-EGF and attenuates cardiac hypertrophy,
suggesting a therapeutic role for this agent.
In addition, maladaptive LVH in the model was associated
with enhanced interstitial fibrosis and activation
of matrix metalloproteinases (MMPs). MMP activity
was increased in DHF and was normalized by administration
of ARBs. Long-term administration of ARBs also inactivated
collagen type 1 and type 3 production, which may translate
into a reduction in fibrosis with ARB therapy, he
said.
|
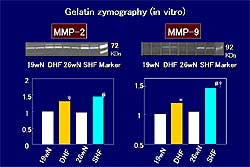 |
| Figure
1. MMP2 activity, but not MMP9 activity, is enhanced
prior to left ventricular dilation. |
| Click
to enlarge |
|
In systolic heart failure (SHF), gelatin zymography
demonstrated enhancement of MMP2 activity before left
ventricular dilatation, which was suppressed by chronic
ACE inhibition, but no enhancement of MMP9 activity
(Figure
1). After LV dilatation, both MMP2 and MMP9 were
activated; ACE inhibition suppressed both MMP2 and
MMP9 and prevented LV remodeling. “Thus, MMP9
rather than MMP2 may be involved in LV dilatation
in SHF and could be a target for preventing LV remodeling,”
he said.
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2003
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|