 |
|
|
 |
| Characteristics of Atherosclerosis
in Japanese: From Genes to Therapy |
|
|
|
 |
|
Risk
Factors for Coronary Atherosclerosis in Recent Japanese
Population Study: Hisayama Study Based on Pathological
Assessment
Yutaka Nakashima
Graduate School of Medical Sciences
Kyushu University, Fukuoka, Japan
|
|
Autopsy data from patients in a long-term observational
study identified age, hypertension, hyperlipidemia,
obesity, and glucose intolerance to be closely related
to coronary atherosclerosis in the Japanese. Although
cerebrovascular diseases have decreased in Japan,
from treatment of hypertension, coronary artery disease
(CAD) is increasing from the Westernization of the
Japanese lifestyle.
The 40-year-old Hisayama study investigated recent
risk factors for coronary atherosclerosis in the Japanese
using a population-based consecutive autopsy series
in people from the city of Hisayama, Japan, near Fukuoka,
and developed a method for the global assessment of
coronary atherosclerosis.
In this series, autopsy was performed on 233 Hisayama
residents who had a medical exam in 1988 (80.9% participation)
and died during the 8-year follow-up period (79.1%
participation). This series is comprised of 125 men,
aged 44-94 years with a mean age of 72 years, and
108 women, aged 46-96 years with a mean age of 74
years. Risk factors studied were: systolic blood pressure
(SBP), diastolic blood pressure, body mass index,
waist-to-hip ratio, serum total cholesterol, HDL cholesterol,
hemoglobin A1c, smoking habit, daily alcohol intake.
|
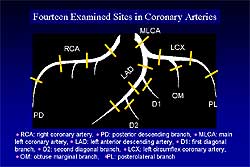 |
| Figure
1. Sites examined to determine degree of coronary
atherosclerosis. |
| Click
to enlarge |
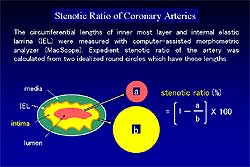 |
| Figure
2. Method used to determine degree of coronary
atherosclerosis. |
| Click
to enlarge |
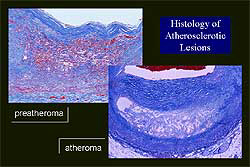 |
| Figure
3. Histological representations of pre-atheroma
and atheroma, the two types of atherosclerosis
on histology. |
| Click
to enlarge |
|
The 14 sites examined in the coronary arteries, selected
on the basis of the AHA reporting system to ensure
thorough study of the atherosclerosis, are shown in
Figure
1. The degree of atherosclerosis is determined
based on histological changes and stenotic ratio,
determined as illustrated in Figure
2. Vessels are photographed on autopsy and computer-corrected
into circles for measurements to determine the stenotic
ratio. The two types of atherosclerosis on histology
are pre-atheroma, an accumulation of foam cells with
adhesion of lipids in the extracellular regions, and
atheroma, necrotic tissue covered by a fibrous cap
(Figure
3). One characteristic of the atheroma in Japanese
is severe fibrotic changes, with limited lipid deposition.
The grading system used in the global assessment of
coronary atherosclerosis is illustrated in Figure
4.
The prevalence of coronary atherosclerosis by grade
and age is shown in Figure
5. Women less than 60 years had milder atherosclerosis,
but after 60 years, the prevalence was similar for
women and men. The incidence of ischemic heart disease
was rare before menopause, but increased, along with
its morbidity, after menopause.
Risk factors for coronary atherosclerosis in men were
SBP, waist-to-hip ratio body mass index, serum total
cholesterol, and hemoglobin A1c. In women the risk
factors were SBP, waist-to-hip ratio body mass index,
and HDL cholesterol, on age-adjusted regression analysis.
Smoking and alcohol intake were not significant risk
factors for coronary atherosclerosis. Stepwise multiple
regression analysis revealed risk factors for men
were age, SBP, serum total cholesterol, and hemoglobin
A1c, and for women were age, SBP, and waist-to-hip
ratio.
|
|
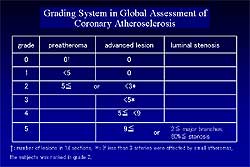 |
| Figure
4. The grading system used for the global assessment
of coronary atherosclerosis in this study. Grade
1 has less than 5 pre-atheroma of 14 sites examined,
Grade 4 has 5-9 atheroma lesions. Grade 5 has
advanced lesions at more than 9 sites or at least
2 major branches with 80% or greater luminal stenosis.)
|
| Click
to enlarge |
|
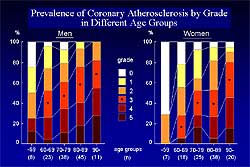 |
| Figure
5.The prevalence of coronary atherosclerosis by
age and grade. More atherosclerotic lesions are
seen with increasing age. The increasing grades
of stenosis are indicated by increasingly darker
colors in the bar graphs. |
| Click
to enlarge |
|
PAGE
TOP
|
Comparison
of the Effects of Beta-Blockers and Calcium Antagonists
on Cardiovascular Events after Acute Myocardial Infarction
in Japanese
Hisao Ogawa
Kumamoto University School of Medicine, Kumamoto, Japan
|
|
The higher incidence of coronary spasm in Japanese
compared to Caucasians is established. About 40% of
patients with angina pectoris and 60% of patients
with organic angina in Japan have coronary spasm.
Sasayama and colleagues have shown a greater incidence
of coronary spasm after acute myocardial infarction
(AMI) in Japanese compared to Caucasians.
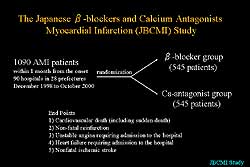
The Japanese Beta-blockers Calcium Antagonists Myocardial
Infarction (JBMCI) study compared the effects of ß-blockers
and calcium channel blockers (CCB) on cardiovascular
(CV) events after AMI, in a multicenter, open-label,
controlled, randomized trial. The benefit of ß-blockers
in AMI has been established, but that of calcium antagonists
has not. Yasue and co-workers showed that CCB effectively
suppress coronary spasm, particularly during exercise,
but ß-blockers aggravate the attacks in some
AMI patients. In the Japanese Antiplatelet Myocardial
Infarction Study (JAMIS) 2 study by Yasue, about 80%
of patients has a CCB and 5% a ß-blocker.
The design of the JBCMI study is outlined in Figure
1. From 1998 to 2000, 1,090 patients were randomized
to ß-blockers or CCB (545 in each group). The
primary endpoints were CV death including sudden death;
nonfatal reinfarction, unstable angina requiring readmission,
heart failure requiring readmission, and nonfatal
ischemic stroke.
The ß-blockers administered were carvedilol
in 310 patients, bisoprolol 138 patients, atenolol
59 patients, and metoprolol 38 patients. CCB were
amlodipine in 469 patients, nifedipine 61 patients,
manidipine 14 patients, and nisolopine 1 patient.
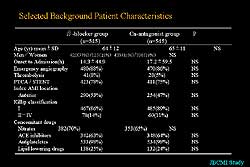
The mean age was 64 years and time from onset to admission
was 14-17 hours. Baseline characteristics are outlined
in Figure
2.
|
|
 |
|
Figure 1. Design of the Japanese Beta-blockers
Calcium Antagonists Myocardial Infarction (JBCMI)
study. |
| Click
to enlarge |
|
 |
|
Figure 2. The baseline characteristics of the
patients in the JBCMI trial. |
| Click
to enlarge |
|
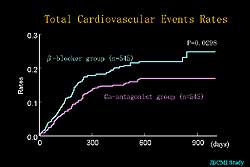 |
| Figure
3. The incidence of total cardiovascular events,
defined as cardiovascular death, reinfarction,
uncontrolled unstable angina, and nonfatal ischemic
stroke in the JBCMI study. |
| Click
to enlarge |
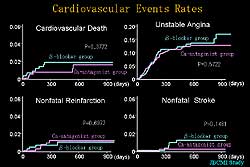 |
|
Figure 4. The incidence of the individual endpoints
in the JBCMI study. |
| Click
to enlarge |
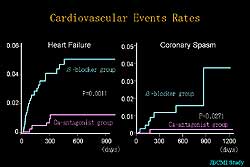 |
| Figure
5. The incidence of heart failure and coronary
spasm were reduced with calcium antagonists compared
to beta blockers. |
| Click
to enlarge |
|
During the mean follow-up of 455 days, the incidence
of total CV events, defined as CV death, reinfarction,
uncontrolled unstable angina, and nonfatal ischemic
stroke, was higher in the ß-blocker group compared
to the CCB group (101 vs 78 events, p=0.0298) (Figure
3). The incidence of heart failure was significantly
higher in the ß-blocker group than in the CCB
group (23 vs 6, p=0.0011) (Figure
4). Coronary spasm was higher in the ß-blocker
group than in the CCB group (7 vs 1, p=0.0271). Because
patients with coronary spasm are readmitted to the
hospital for refractory chest pain, this number may
exclude the cases of mild coronary spasm responding
to drug therapy, said Hisao Ogawa of Kumamoto University
School of Medicine, a study investigator. The onset
of coronary spasm was delayed with CCB but not with
ß-blocker (Figure
5).
In summary, the incidence of coronary spasm was 40.2%
in 2195 consecutive patients with angina pectoris
in this multicenter study in Japan. CCB may be more
useful than ß-blockers for AMI in Japanese patients,
especially for the prevention of heart failure and
coronary spasm. However, CV events other than heart
failure, including cardiac death and refractory angina,
were the same in the two groups. ß-blockers are beneficial
in patients with left ventricular dysfunction after
AMI. Thus, in patients with AMI, ß-blockers should
be carefully administered with small initial doses
with more gradual dose titration. In the absence of
heart failure, a usual starting dose may be initiated.
|
PAGE
TOP
|
Importance
of Rho-Kinase in the Pathogenesis of Arteriosclerotic
Vascular Disease in Japanese
Hiroaki Shimokawa
Kyushu University Graduate School
of Medicine, Fukuoka, Japan
|
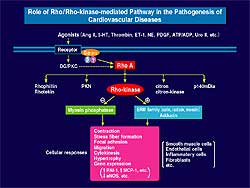 |
| Figure
1. The Rho/Rho kinase pathway suppresses myosin
phosphotase and increases vessel calcium sensitivity.
Target proteins affect contraction, stress fiber
formation, focal adhesion, migration, cytokinesis,
cell hypertrophy, and gene expression. G-protein
coupled agonists are involved in the pathogenesis
of atherosclerosis. |
| Click
to enlarge |
|
The Rho/Rho-kinase pathway is involved in the development
of cardiovascular (CV) diseases (Figure
1). Research by Hiroaki Shimokawa and colleagues
at Kyushu University Graduate School of Medicine shows
that Rho-kinase may be involved in spasm-related diseases
of the vessel and the development of atherosclerosis.
Coronary inflammation changes at the adventitia is
seen in persons who die from coronary spasm. In the
porcine model given microbeads with the inflammatory
cytokine IL-1ß, this group showed serotonin-induced
enhanced coronary artery spasm. This porcine model
was used to study the changes in the Rho-kinase pathway,
in which the expression of Rho mRNA is enhanced. Rho-kinase
has 3 domains, catalytic, coiled-coil, and PH, with
a Rho-binding (RB) domain at the coiled-coil domain.
Rho-kinase activity is blocked by overexpression of
the RB-PH domains.
Fasudil, approved for coronary spasm, is metabolized
by the liver into hydroxyfasudil, which is highly
selective for blocking Rho-kinase. In the porcine
model with IL-1ß, hydroxyfasudil suppressed
serotonin-induced coronary spasm in a dose-dependent
manner, but not coronary spasm in normal coronary
arteries.
|
 |
|
Figure 2. The molecular mechanisms for coronary
vascular spasm. |
| Click
to enlarge |
|
The myosin binding subunit of myosin phosphatase
is phosphorylated and inactivated by Rho-kinase, showing
a Rho-kinase activity. The Rho-kinase inhibitors,
fasudil and Y-27632 suppressed the enhanced Rho-kinase
activity in the porcine model of coronary spasm/arteriosclerosis.
The close correlation between the Rho-kinase and coronary
spasm supports the involvement of Rho-kinase in the
pathogenesis of coronary spasm.
The mechanisms for coronary spasm include suppression
of myosin phosphotase and resultant enhancement of
myosin phosphorylation (Figure
2). Interaction with actins induces vascular spasm.
Rho-kinase expression is increased in inflammatory
atherosclerotic lesions
In humans, fasudil suppresses acetylcholine-induced
focal spasm, but not normal coronary artery constrictions.
Fasudil also suppresses the incidence of diffuse multivessel
spasm in patients with vasospastic angina.
|
|
Pokkuri disease, or sudden nocturnal death, occurs
in persons with no previous sign of disease. A comparison
of the lipid profiles in persons who died from Pokkuri
disease and from accidents showed that the triglyceride
level and particularly remnant lipoprotein triglyceride
level (RLP-TG) are very high in Pokkuri disease. Pokkuri
disease and coronary spasm are more frequent in the
early morning and in Asian males. RLP-TG might be
associated with both.
A comparison of Pokkuri-derived RLP fractions and
bound fractions showed that serotonin caused a severe
contraction only at the coronary segments treated
with RLP fraction. This was significantly suppressed
with the pre-administration of the Rho-kinase inhibitor,
hydroxyfasudil, in the porcine model. Rho-kinase expression
is significantly enhanced in the RLP fractions compared
to the bound fractions from patients with Pokkuri
disease. A high level of RLP may induce fatal coronary
spasm, stated Shimokawa.
Atherosclerosis and Rho-kinase
Rho-kinase down regulates eNOS, BMP-2, and
osteocalcin, which are said to suppress atherosclerosis.
In contrast, Rho-kinase upregulates MCP-1, PAI-1,
tissue factor, TGF-ß1, collagen I, IL-6, Rho-kinase,
NAD(P)H, MIF, and IFN- . .
In a balloon injury porcine model, pre-administration
of Rho-kinase prevented atherosclerotic changes. MCP-1
induces atherosclerotic lesions, but fasudil suppresses
this action. Also, some studies have shown that Rho-kinase
inhibitors may prevent atherosclerosis after heart
and liver transplantation.
Long-term inhibition of Rho-kinase can eliminate the
constrictive remodeling of the porcine coronary artery.
Constrictive remodeling occurs at the inflammatory
coronary lesions, but the transfection of dominant-negative
Rho-kinase regresses the remodeling, as shown by increased
luminal cross-sectional area on angiography.
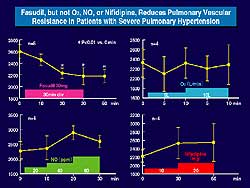
Pulmonary hypertension and Rho-kinase
Although the pathophysiology of pulmonary
hypertension is unclear, Rho-kinase is thought to
be involved with the inflammatory and proliferative
changes of the pulmonary arteries that may lead to
proliferation and hypertrophy, adhesion and migration
of the inflammatory cells, injury and thrombosis of
endothelium, and hypercontraction of vascular smooth
muscle cells.
In the pulmonary hypertensive rat model, severe pulmonary
hypertension was established 3 weeks after injection
of monocrotaline (MCT). When untreated, 80% of the
rats died within 8 weeks. Survival is improved with
long-term oral treatment with fasudil. Further, fasudil
improved survival even after pulmonary hypertension
was established. The Rho-kinase inhibitor improves
pulmonary vascular lesions and right ventricular hypertrophy
in pulmonary hypertension. Fasudil, but not nitric
oxide or nifedipine, reduced vascular resistance in
patients with severe pulmonary hypertension (Figure
3).
In summary, Rho-kinase is a therapeutic target, whose
inhibitors have been shown to be effective for cerebral
vasospasm, coronary artery spasm, hypertension, pulmonary
hypertension, and sudden death (Figure
4). Atherosclerotic diseases, such as angina,
myocardial infarction, restenosis, coronary artery
dysfunction after transplantation may be treated by
targeting Rho-kinase.
|
|
 |
|
Figure 3. Vascular resistance in pulmonary hypertension
is improved with fasudil, the Rho kinase inhibitor,
but not with nitric oxide or nifedipine. |
| Click
to enlarge |
|
|
PAGE
TOP
|
G (-670) A Polymorphism in the Promoter Region of the Fas Gene is a Risk Factor for Myocardial Infarction
Keisuke Fukuo
Osaka University Medical School, Osaka, Japan
|
|
Fas is a member of the TNF- receptor family. Binding to the Fas ligand activates
apoptosis-related enzymes such as caspase. Although
Fas is expressed in most cell types, Fas ligand (FasL)
is expressed only in natural killer cells, activated
T cells, macrophages, and other immune and inflammatory
cells. When the FasL is cut off from the membrane
by metalloproteinase, it becomes soluble (sFas), which
may be involved in the induction of the inflammatory
reactions and other apoptotic activity, explained
Keisuke Fukuo, Osaka University Medical School.
receptor family. Binding to the Fas ligand activates
apoptosis-related enzymes such as caspase. Although
Fas is expressed in most cell types, Fas ligand (FasL)
is expressed only in natural killer cells, activated
T cells, macrophages, and other immune and inflammatory
cells. When the FasL is cut off from the membrane
by metalloproteinase, it becomes soluble (sFas), which
may be involved in the induction of the inflammatory
reactions and other apoptotic activity, explained
Keisuke Fukuo, Osaka University Medical School.
The role of the Fas/FasL system in atherogenesis is
being elucidated by work from this group and others.
Atherogenic factors such as oxidative stress induces
endothelial cell apoptosis via Fas-mediated pathways.
Fas-mediated vascular smooth muscle cell apoptosis
may exaggerate plaque vulnerability via induction
of inflammation. FasL expressed in endothelial cells
may regulate the accumulation of inflammatory cells
into the vessel wall. Soluble fasL (SfasL) released
from endothelial cells may protect against hypoxia-induced
endothelial cell apoptosis. Plasma sFasL levels are
increased in patients with heart failure and acute
coronary syndrome. Fas-mediated apoptosis may serve
as a negative feed back mechanism for the elimination
of activated macrophages in the vessel wall.
Infiltration of inflammatory cells into endothelium
causes plaque instability and is related to the development
of cardiovascular (CV) events. The mechanisms for
the accumulation of macrophages in the vessel wall
may include MCP-1, which may be related to the migration
or chemotaxis, proliferation, and apoptosis. This
group showed in mice studies that activated macrophages
cause apoptosis in control mice, but not in Fas-lacking
mouse. The macrophage accumulation in the perivascular
space is greater in the Fas-lacking mice than in controls.
Work by this group and others has shown the following.
The atherogenic diet induced vasculitis, lipid accumulation,
and a higher incidence of myocardial infarction (MI)
in Fas-lacking mice compared to controls. Mutations
in the Fas gene were associated with autoimmune disease.
Importantly, patients with SLE and other autoimmune
disease are associated with a higher CV mortality.
Fas signaling is required in the compensation of pressure
overload, and its absence leads to rapid ventricular
dilation, failure and increased mortality, without
compensatory hypertrophy. Thus, abnormality of the
Fas gene may be a genetic risk factor for CV disease.
Fas gene polymorphism and MI
This group conducted a study to assess
whether a polymorphism in the promoter region of the
Fas gene is associated with an increased risk for
MI in Japanese subjects. Two polymorphisms have been
identified in the promoter region of the Fas gene.
The single base change from GA to GG was the focus
of this presentation.
The TaqMan (the fluorogenic 5’ nuclease polymerase
change reaction)-PCR method was used. Six hundred
sixteen patients were studied (AMI positive 154, AMI
negative 462), with a mean age of 63 years (82% male
in both groups). Smoking (61% vs 38%), hypertension
(52% vs 40%), diabetes (36%vs 8%), and hyperlipidemia
(48% vs 22%) were greater in the AMI positive than
the AMI negative patients.
No age or sex difference in the 3 groups based on
the polymorphism. However, the incidence of MI was
higher in the AA group compared to the GA and GG groups
(35%, 23%, 19%, respectively). An A allele is associated
with an odds ratio of 2.62 for an MI, and it is an
independent risk factor for MI, based on logistic
regression analysis.
JAK and STAT seem to be stimulated in the system regulating
Fas expression. STAT3 is reported to have a negative
effect on FAS expression. The GAS region is the dominant
binding region. A GAS sequence is present in patients
with an A allele, but not those with a G allele. In
A allele patients, Fas expression is suppressed by
GAS sequence-stimulation of STAT3. This does not occur
in G allele patients.
Leukemia inhibitory factor (LIF), an activator of
STAT3, suppressed Fas expression in the AA genotype
but not in the GG genotype in an experiment by this
group. Further work showed that LIF suppressed the
promoter activity in Cos 7 cells transfected with
the construct containing AA but not GG genotype. Hence,
the difference in genotype seems to be related to
the difference in transcription activity.
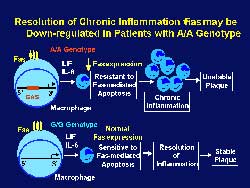
In patients with the AA genotype, there are 3 defects
in the GAS sequence. Cytokine stimulation of STAT3
suppresses Fas expression, leading to Fas-mediated
apoptosis.
Thus, the mechanism to eliminate inflammatory cells
from the endothelium is weakened or suppressed, causing
unstable plaque formation. The lack of a GAS sequence
in the GG phenotype means no stimulation of STAT3
and suppression of Fas expression, allowing inflammatory
cells to be eliminated from the endothelium, making
the plaque more stable (Figure
1).
In conclusion, the A allele of the GA polymorphism
in the promoter region of the Fas gene may be a new
genetic risk factor for MI via downregulation of Fas
expression.
|
 |
|
Figure 1. Differential regulation in patients
with the AA and GG phenotypes and its effect on
plaque stability. |
| Click
to enlarge |
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2003
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|