 |
|
|
 |
| Progress in the Pathophysiology
and Treatment of Pulmonary Hypertension |
|
|
|
 |
|
Possible
Effectiveness of Combination Therapy in Patients with
Severe Pulmonary Hypertension
Masahito Sakuma
Tohoku University Graduate School
of Medicine, Sendai, Japan
|
|
Previous work by this group showed that epoprostenol
(Epo) was associated with a satisfactory response
in 44.4% of treated patients with pulmonary hypertension
(PH) and NYHA class I and mild NYHA class II heart
failure. An unsatisfactory response was seen 38.9%
of patients and early death in 16.7% of patients.
This indicates that chronic Epo therapy improves quality
of life but not does not improve clinical status in
one-half of patients. Nitric oxide (NO) inhalation
is another important therapeutic tool of PH. NO inhalation
has been shown to reduce right arterial pressure and
increase cardiac output.
This group investigated the feasibility of combination
therapy of Epo and NO inhalation for primary pulmonary
hypertension (PPH), by assessing inhaled NO levels
in patients with PH treated chronically with Epo.
Protocol 1 examined the hemodynamic effects in 10
patients with PPH (age 34 years±10.7 years;
2 males) after chronic treatment with Epo (32.0±15.8
ng/kg/min) for 19.1±15.6 months. NO inhalation
was performed during catheterization. Mean pulmonary
artery pressure and right artery pressure were significantly
reduced (54.9 to 51.9 mm Hg, p=0.02; 8.5 to 7.0 mm
Hg, p=0.02, respectively). Cardiac output increased
from 4.56 to 5.04 (p=0.03) and pulmonary vascular
resistance decreased from 905 to 733 (p=0.005). The
ratio of pulmonary vascular to systolic vascular resistance
was reduced from 0.63 to 0.57 (p=0.01).
Protocol 2 compared the hemodynamic effect of NO inhalation
before and after chronic treatment with Epo. Six women
with PPH (age range 24 to 53 years) were treated with
Epo (dose range 17.3-49 ng/kg/min) for 3 to 24 months.
Cardiac output and heart rate were increased after
chronic treatment with Epo. Pulmonary vascular resistance
was significantly reduced from 1.2% before Epo therapy
to minus 18.95 after Epo therapy (p<0.05).
The investigators conclude that NO inhalation has
an additional effect on the pulmonary circulation
during chronic use of Epo and this suggests that Epo
improves pulmonary vascular responsiveness to NO inhalation.
The combination of Epo infusion and augmentation of
NO or the effects of NO (NO inhalation, NO donor or
phosphodiesterase V inhibitor which enhances the effects
of both intrinsic and extrinsic NO) might improve
the prognosis in patients with PH more than either
therapy alone. The best combination therapy for PH
must be examined in addition to assessing newer medications.
|
PAGE
TOP
|
Inhibition
of Type 5 Phosphodiesterase: Promising Therapy for
Pulmonary Hypertension
Hiroshi Watanabe
Hamamatsu University School of
Medicine, Hamamatsu, Japan
|
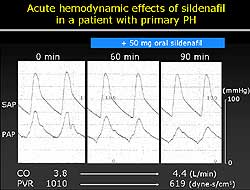 |
| Figure
2. The acute hemodynamic effects of sildenafil
in a patient with primary pulmonary hypertension. |
| Click
to enlarge |
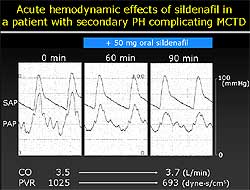 |
| Figure
3. The acute hemodynamic effects of sildenafil
in a patient with secondary pulmonary hypertension. |
| Click
to enlarge |
|
Oral sildenafil, a type 5 phosphodiesterase inhibitor,
may be valuable as a vasodilator in patients with
primary and secondary pulmonary hypertension, according
to a study performed at Hamamatsu University School
of Medicine. Figure
1 illustrates the role of sildenafil in regulating
vascular tone.
The study examined the hemodynamic efficacy and safety
of short- and long-term treatment with sildenafil
in 10 patients with primary and secondary pulmonary
hypertension: 2 with primary pulmonary hypertension,
5 with connective tissue disease, and 3 with congenital
heart disease. Patients received sildenafil 50 mg
orally during cardiac catheterization. Pulmonary arterial
pressure, systemic arterial pressure, cardiac output
and other parameters were measured before and after
sildenafil administration. Patients who had a positive
hemodynamic response were then maintained on sildenafil
25 mg orally BID. Long-term hemodynamic effects were
evaluated by repeat cardiac catheterization after
3 months.
Seven of the 10 patients responded to sildenafil.
After the first administration, sildenafil decreased
mean pulmonary arterial pressure by 27%, increased
cardiac index by 18%, and reduced pulmonary artery
resistance by 41%. It did not affect systemic artery
pressure, reported Watanabe. Figure
2 shows the acute dynamic effects of sildenafil
in a patient with primary pulmonary hypertension,
and Figure
3 illustrates this in a patient with secondary
pulmonary hypertension.
After 3 months of treatment, sildenafil increased
cardiac index by 15%, reduced mean pulmonary arterial
pressure by 26%, and reduced pulmonary artery resistance
by 37%.
“The responders were maintained on 24 mg oral
sildenafil twice a day with remarkable improvement,”
he said. New York Heart Association functional class
returned from III to II, and serum brain natriuretic
peptide (BNP) levels dropped by 50%. Follow-up cardiac
catheterization after 3 months showed that the hemodynamic
efficacy of sildenafil was well-preserved.
|
|
The 3 nonresponders were patients with congenital
heart disease who had secondary pulmonary hypertension
for more than a decade and demonstrated mean arterial
pressures of more than 70 mm Hg. “These probably
are the factors that limited the efficacy of sildenafil,”
Watanabe said.
“The results of this study indicate that sildenafil
satisfies the recommended criteria for an agent to
treat pulmonary hypertension, which includes a more
than 25% reduction in mean pulmonary arterial pressure
and a 33% fall in pulmonary vascular resistance,”
he concluded. Positive responses to vasodilating agents
in pulmonary hypertension are known to improve long-term
clinical outcomes. The data presented suggest that
oral sildenafil may be a valuable vasodilator in patients
with primary and secondary pulmonary hypertension.
Although the twice-daily dosing was effective, longer-acting
formulations may be needed for more stable control
of pulmonary artery pressure.
|
PAGE
TOP
|
Living-Donor
Lobar Lung Transplantation for End-Stage Primary Pulmonary
Hypertension
Hiroshi Date
Okayama University Graduate School
of Medicine and Dentistry, Okayama, Japan
|
|
In living-donor lobar lung transplantation (LDLLT),
an alternative to cadaver lung transplantation, two
healthy donors donate the right or left lower lobe
of their lung and these are transplanted into a recipient
as a whole right and left lung. Because of the limited
amount of lung tissue that is transplanted in this
procedure, it is best suited to children or adults
who are small in size. It has been most exclusively
performed for cystic fibrosis. Although LDLLT has
been successfully performed in pediatric primary pulmonary
hypertension (PPH), its use in adult PPH has not been
proven.
These investigators evaluated the effects of LDLLT
for pediatric and adult patients with end-stage PPH.
From January 2001 to December 2002, 9 patients were
studied (2 male, 7 female; average age 19 years, range
8-31 years; 4 children, 5 adults). This group has
successfully used LDLLT in 11 other patients with
other indications. Currently all patients are still
living. Eight of the patients had bilateral transplantation,
while 1 child had unilateral transplantation, because
the mother was the only available donor. All 17 donors
(7 fathers, 6 mothers, 4 brothers) have returned to
their normal daily life. The mean graft size was 69.9±5.5%
of the predicted value of the recipient.
The pathology of the excised lungs was PPH in 7 patients
(H-E grade 3 in 1 patient, H-E grade 6 in 6 patients),
pulmonary capillary hemangiomatosis in 1 patient,
and pulmonary veno-occlusive disease in 1 patient.
At 2 to 3 months post-transplant, mean pulmonary arterial
pressure was reduced from 61.7±5 mm Hg pre-transplant
to 16.1±1.8 mm Hg (p=0.0001). Cardiac index
increased from 1.9±0.1 L/min/m2 pre-transplant
to 2.9±0.2 post-transplant (p=0.0001). The
reduced pulmonary arterial pressure was sustained
at 1 year, while the cardiac index was further improved
(Figure
1). The changes on chest x-ray in 1 recipient
is shown in Figure
2. Pulmonary function testing showed steady improvement
during the first year, with forced vital capacity
reaching 2000 ml (17% of predicted value).
|
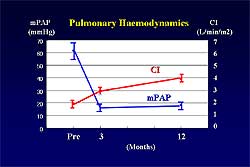 |
| Figure
1. In 9 patients receiving LDLLT, improvement
in the mean pulmonary arterial pressure is maintained
while the cardiac index is further improved. |
| Click
to enlarge |
|
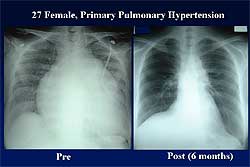 |
| Figure
2. The changes seen on chest x-ray post-transplant
compared to pre-transplant in one LDLLT recipient.
|
| Click
to enlarge |
|
PAGE
TOP
|
Rho-Kinase
is an Important Therapeutic Target for the Treatment
of Pulmonary Hypertension
Kohtaro Abe
Kyushu University Graduate School
of Medicine, Fukuoka, Japan
|
|
This group recently demonstrated that Rho-kinase,
a target of the small GTPase Rho, is substantially
involved in the pathogenesis of arteriosclerosis in
animal models. They propose that this mechanism may
also be involved in primary pulmonary hypertension
(PPH).
In adult male Sprague-Dawley rat model of monocrotaline-
(MCT) induced PPH, 4 groups were studied (control,
MCT, prevention protocol (fasudil treatment from day
0), treatment protocol (fasudil treatment from day
21). Fasudil is a long-term oral treatment that is
metabolized to hydroxyfasudil, a specific Rho-kinase
inhibitor.
In the prevention protocol, survival was very poor
in the monocrotaline group (27%) while it was greatly
improved in the low dose (83%) and high dose (93%)
fasudil groups. In the treatment protocol, even though
treatment began after the establishment of PPH, fasudil
significantly and dose-dependently improved prognosis
(43% low dose, 86% high dose) compared to the MCT
group.
Fasudil prevented MCT-induced PH and right ventricular
(RV) hypertrophy at day 21 and day 63 in the prevention
group. Clinically important, fasudil caused a marked
regression of MCT-induced PH and RV hypertrophy in
the treatment group. Histology showed that medial
wall thickening seen in the MCT group was markedly
suppressed in the fasudil-treated groups in both protocols.
Pulmonary vascular lesion formation was prevented
or markedly regressed with fasudil.
In terms of mechanisms, long-term fasudil treatment
in the prevention protocol was associated with 1)
suppression of MCT-induced vascular smooth muscle
(VSMC) proliferation, 2) macrophage accumulation,
3) enhanced apoptosis of VSMC, 4) prevention of MCT-induced
endothelial dysfunction of pulmonary arteries, 5)
suppression of MCT-induced VSMC hypercontractions
in response to serotonin, 6) significant suppression
of MCT-induced Rho-kinase activity, and 7) upregulation
of eNOS in the lungs.
Hence, these results demonstrate the proliferation
and hypertrophy of VSMC, adhesion and migration of
inflammatory cells, injury and thrombosis of the endothelium,
and hypercontraction of VSMC—all of these mechanisms
are involved in the pathogenesis of MCT-induced PH
in rats. They further demonstrated that inhibition
of Rho-kinase is effective for the prevention and
treatment of PH in this model.
In a clinical study of 10 patients with severe PH
(3 primary, 7 secondary), they showed that 30-minute
intravenous fasudil treatment did not affect pulmonary
artery pressure, nor did oxygen inhalation, nitric
oxide inhalation, or nifedipine. Pulmonary vascular
resistance was not ameliorated by oxygen inhalation,
nitric oxide inhalation, or nifedipine, but was significantly
suppressed by fasudil. Systemic hypertension was not
induced by fasudil treatment.
Their work shows that Rho-kinase is substantially
involved in the pathogenesis of MCT-induced and hypoxia-induced
PH (shown in a separate study) in rats. Rho-kinase
may also be involved in the pathogenesis of PH in
humans. Rho-kinase may be a novel therapeutic target
in the treatment of PH.
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2003
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|