 |
|
|
 |
| Physical Therapy for Heart Failure |
|
|
|
 |
|
Mechanisms of Improvement to Myocardial Perfusion after Exercise Training in Ischemic Cardiomyopathy
Romualdo Belardinelli
ULancisi Heart Institute, Ancona, Italy
|
|
Accumulating evidence shows that exercise may have
therapeutic benefits in heart failure, beyond being
a stressor useful for diagnostic purposes. An inverse
correlation between the level of physical activity
(the fitness level) and the level of events and survival
was found in an analysis of 1000 normal patients in
randomized trials. In short, survival was best in
the persons who were more active.
Myers and colleagues reported that in 7,600 males
with and without cardiovascular (CV) disease that
the higher level of exercise capacity the lower the
risk of death. A peak oxygen uptake above 30 was associated
with a 5-fold less risk of death compared to a peak
oxygen uptake less than 30, independent of the presence
or absence of CV disease.
Factors predictive of improvement in functional
capacity after exercise training (ET) in chronic heart
failure patients (CHF) include a low peak VO2 (<14
mL/kg/min), an abnormal relaxation pattern of left
ventricular (LV) diastolic filling, a normal cardiac
output/workrate slope, hibernating “viable “
myocardium, BMI <30, and male sex. This suggests
that with the presence of abnormalities in the heart
and pulmonary circulation, there would be less chance
to improve functional capacity in these patients.
Thus, based on these studies, the periphery seems
to be less important than these central factors.
|
|
Improved myocardial perfusion
Myocardial perfusion can be improved with 8-weeks
of ET. Improvement in myocardial perfusion can translate
into better survival. For example, in a patient with
ischemic cardiomyopathy (ICM), before ET there was
a clear abnormality in the ECG suggesting myocardial
ischemia with stable angina, and at the end of the
8-week ET the ECG was normal, an improvement in myocardial
scintigraphy. This was an intriguing observation.
The number of viable segments before ET was predictive
of the functional capacity in patients exercised at
60% of peak oxygen uptake for 8-weeks, in a 1998 report
by Belardinelli and colleagues. Functional capacity
was improved after 8-weeks ET in the patients with
improved contractility with a low-dose dobutamine
stress echocardiography, improved LV ejection fraction
(LVEF), and systolic wall thickness core index. Thus,
identifying hibernating myocardium before ET may be
predictive of improvement in functional capacity and
myocardial perfusion in patients with ICM.
|
|
Oxidative stress and exercise
Exercise may be an important tool, but the type,
intensity, and the modality of exercise must be considered.
Physical exercise may determine oxidative stress,
and a high level of oxidative stress is associated
with endothelial dysfunction, which can result in
a less marked improvement of functional capacity.
A low or normal level of oxidative stress is associated
with absent or mild endothelial dysfunction and greater
improvement in functional capacity. For example, in
a patient with hypercholesterolemia, after 30 minutes
of acute exercise, in the high intensity group (80%
of VO2 max) there was a paradoxical 25% reduction
in the flow-mediated dilation of the brachial artery,
while in the mild intensity group (40% VO2 max) there
was a marked 90% improvement in flow-mediated dilation.
These changes were correlated to oxidative stress,
as measured by plasma malondealdehyde, which was markedly
increased in the high intensity group (from about
30 to 50 nmol/mL) and not increased in the low intensity
group (about 25 nmol/mL).
In another study, they tested the oxidative stress
after eccentric exercise, known to be a greater stimulator
of oxidative stress, and found that in patients with
ICM the increase in plasma malondealdehyde was earlier
after eccentric exercise compared to in healthy subjects.
But, exercise may also induce important adaptation
in the heart and vessel. Genes coding anti-oxidant
enzymes are over-expressed by a program of ET in patients
with CHF. Researchers from France showed that the
gene of nitric oxide synthase and superoxide dysmutase
is increased by ET, suggesting that an improvement
in endothelial function may play an important role.
Brown and colleagues showed that when looking at
coronary internal dimensions and flow resistance during
isometric exercise, with handgrip there was a 10%
reduction in the luminal area. In the presence of
coronary stenosis this can cause myocardial ischemia.
But for handgrip plus nitroglycerin, there was dilation
of the coronary artery (about 30% increase in luminal
area), which was about the same level with sublingual
nitroglycerin. So, this is an important concept to
consider when exercising patients with coronary stenosis.
Nitric oxide was found to be involved in this reaction.
Gordon and colleagues showed that during aerobic exercise
in the presence of coronary artery stenosis there
is a tendency towards a constriction of the segments
with mild stenosis or more severe stenosis, which
behaves as it would after administration of acetylcholine.
Importantly, post-exercise constriction is likely
related to a lack of nitric oxide. After atrial pacing,
normal coronary artery segments dilate, but pre-stenotic
and stenotic vessels are narrowed, meaning myocardial
perfusion may be deteriorated in those segments.
So, different problems are present. Exercise and
myocardial perfusion in the coronary vessels is related
to the presence or absence of abnormalities in the
vessels. The abnormalities may be anatomical (stenosis),
functional (vasomotor tone, endothelial dysfunction,
autonomic imbalance) or both. The myocardium may be
normal, or coupled with varying amounts of abnormal
myocardium (necrotic, stunned, hibernating, fibrotic).
These may be 4 models that may be seen frequently
in clinical practice. For example, a patient may have
single vessel disease with stunned myocardium, or
multiple vessel disease with stunned myocardium, or
single vessel disease with necrotic area and hibernating
myocardium, or multiple vessel disease with necrotic
area and hibernating stunned myocardium. This may
affect the response to ET.
Work by White and colleagues reported in 1993 showed
that after ameroid occlusion of the left circumflex
in the porcine model that 4 weeks of ET was associated
with an astonishing increase of the vascularity of
the coronary tree, especially the small vessels, compared
to the control animal. This suggests sort of an angiogenesis
or arteriogenesis can be stimulated by exercise.
In a human model, after gated SPECT and ET (60%
of peak VO2, 3 times per week, 6 months) there was
a dramatic reduction in the perfusion defect in the
septal inferior wall with nearly complete reversibility.
|
|
Hypothesis One
There are several hypotheses that may explain the
improvement of myocardial perfusion in this human
model of ICM. One hypothesis may be coronary stenosis
regression with ET. Hambrecht and colleagues showed
that after a program of aerobic exercise there was
no disease progression in the majority of patients,
and regression in a minority of patients, indicating
that with ET it is possible to obtain a sort of stabilization
of the plaque and possibly an improvement in myocardial
perfusion.
In the SCRIP study in 300 patients followed for
4 years, coronary artery disease (CAD) progression
was reduced by 47% in the multifactorial risk reduction
group, compared to the usual care group. The hospital
readmission rate was 76% in the usual care group.
In the multifactorial risk reduction group, triglycerides
were reduced 20%, total cholesterol 40%, and LDL cholesterol
23.5%, and HDL cholesterol increased 12% and exercise
capacity 20%. There was no change in the parameters
in the usual care group. This suggests that a reduction
in the progression of CAD or regression of CAD may
be a possible explanation.
A study by Belardinelli and colleagues in patients
after PTCA, showed that a 6-month ET program was associated
with a reduction in total cholesterol, smoking, and
triglycerides and an improvement in BMI. In the untrained
patients, a 25% progression of CAD was found, compared
to a 7.6% progression in the trained patients. No
change was found in 89% of the trained patients and
75% of the untrained patients. A 4.4% regression of
CAD was found in the trained patients, compared to
no regression in the untrained patients.
|
|
Hypothesis Two
The second hypothesis is vascular remodeling. The
vascular tree attempts to compensate for problems
in perfusion and is able to react to different stimuli,
for example shear stress or increasing metabolic demand
in ischemic tissue by remodeling. This can lead to
more direct blood flow. In one example, after 6-months
of ET, an improvement in myocardial perfusion and
extension of the defect is reduced by 30%, with remodeling
of the vessel. This also translated into an improvement
in LV function, with EF increasing from 42% to 49%
at the end of the study. Clear improvement in contractility
was seen.
|
|
Hypothesis Three
Belardinelli and colleagues demonstrated that an
improvement in myocardial coronary collateralization
after ET in a model of ICM determines an improvement
in myocardial perfusion. Improvement in contractility
was associated with an improvement in myocardial perfusion,
which was not due to just a peripheral effect of ET,
as shown by the improved systolic blood pressure and
systolic volume inverse relation in the trained patients
versus controls.
Myocardial blood flow is increased in the collateral-dependent
region in part because of an endothelium-dependent
mechanism. This may be evident when the extent of
the infarction is below 50% of the heart. They found
that after ameroid plus 8-week ET, the number of the
small vessels increased. This may be related to a
mechanism of ateriogenesis. In fact, in dogs treated
with FGF and VEGF, they found improved collateral-dependent
blood flow after acute myocardial infarction, which
was in part related to nitric oxide.
Several angiogenic peptides can be involved in this
regulation. These peptides may be different on the
basis of severe coronary artery stenosis. An endothelium-independent
mechanism also plays a role. Work by Symons and colleagues
showed that dipyradimole increases the concentration
of adenosine in the myocardium, and there is an increase
in the transmural coronary blood flow that is not
very different than that obtained from with diltiazem,
an endothelium-independent dilator. In a study by
Belardinelli and colleagues, dipyradimole plus ET
resulted in an additive effect in patients with ICM,
with a greater increase in the coronary collateral
score than in patients treated with dipyradimole alone.
These changes were also associated with improvement
in myocardial perfusion that was more marked in dipyridamole
plus ET compared to dipyradimole alone. Systolic wall
thickness core index was less marked. Improvement
in the collaterals was found that was more evident
in the dipyridamole plus ET group.
Arteriogensis and angiogenesis may be involved in
the same mechanism after ET. Ateriogenesis is defined
as the enlargement of pre-existing collateral arterioles
allowing increased blood flow to downstream tissue.
Angiogenesis is defined as the proliferation of capillaries
within tissue. The stimuli for ateriogenesis are increased
shear stress, while for angiogenesis it is hypoxia/ischemia.
In the model of human ICM studied by Belardinelli,
both ateriogenesis and angiogenesis probably contributed
to an improvement in myocardial perfusion in the tissue.
The mediators for arteriogenesis are MCP-1, TGF-beta,
beta-FGF, PIGF, PDGF, and MMPs, and for angiogenesis
they are TGF-alpha, alpha-FGF, beta-FGF, PIGF, PDGF,
and MMPs. The result of ateriogenesis is remodeling
of aterioles into collateral vessels, and of angiogenesis
is formation of new capillaries.
|
|
Hypothesis Four
Endothelium-dependent dilation is a mechanism that
has been postulated and demonstrated recently. ET
may induce the expression of genes such as nitric
oxide synthase, and may reduce the inactivation of
nitric oxide. These are mechanisms that can contribute
to the increase of the biological activity of nitric
oxide. Hambrecht and colleagues demonstrated that
1-month of ET improved the vasomotor response and
endothelium-dependent response in the treated coronary
artery. Sessa and colleagues demonstrated an increase
in ecNOS expression in animals.
In animals, an increase in myocardial capillary
diffusion capacity after ET has been shown by Laughlin
and colleagues. This likely explained the improvement
in myocardial perfusion in the canine model.
Continued ET is associated with continued improvement
in patients, as shown by Belardinelli and colleagues.
The improvement achieved after 8-week of ET was maintained
at 1 year. Sustaining an improvement in myocardial
perfusion is likely to improve prognosis. Data from
the ETICA study by this group, published in 1999,
showed that improved myocardial perfusion is associated
with an improved prognosis. After coronary angioplasty,
in the training group after 6-months of ET at 60%
of peak VO2, total myocardial perfusion was improved,
which was associated with an improvement in peripheral
endothelial function. Continued ET in these patients
showed progressive improvement over a 6-year period.
Importantly, this means it would be possible to sustain
the improved perfusion. Improved myocardial perfusion
over time is predictive of a better prognosis.
|
|
Conclusion
Chronic exercise may induce structural and functional
adaptation in the coronary vessels that can determine
an improvement in myocardial perfusion. Several mechanisms
may be involved. ET may exert a direct action or an
indirect action. The direct action is mediated by
an increase in shear stress that determines a cascade
of events, and determining an improvement in vasomotor
function. Indirect action is related to an improvement
of the coronary risk profile, especially in patients
with ICM, determining a reduction in arteriosclerosis
progression. The field of exercise-induced improvement
in myocardial perfusion is very intriguing, but a
definitive conclusion in this field has not been achieved
yet.
|
PAGE
TOP
|
Clinical Efficacy and Cost-Benefit Analysis of Nocturnal
Home Oxygen Therapy in Patients with Chronic Heart
Failure and Sleep-Disordered Breathing
Yoshihiko Seino
Nippon Medical School, Tokyo,
Japan
|
|
Evidence that sleep apnea, described as Cheyne-Strokes
respiration, may adversely affect the pathophysiology
and outcomes of chronic heart failure (CHF) is increasing.
Sleep apnea has been suggested as the next therapeutic
target in CHF.
Sleep-disordered breathing (SDB) comprises 2 major
forms in CHF. Obstructive sleep apnea results from
sleep-induced episodes of partial or complete upper
airway collapse. The risk factors for obstructive
sleep apnea differ by gender; an increase in BMI or
obesity in men and age in women. Central sleep apnea
arises from the lack of neuronal impulse to respiratory
muscles. The principle risk factors for central sleep
apnea are male sex, increasing age, hypercapnia, and
atrial fibrillation, but not obesity.
|
|
Cheyne-Stokes respiration
A prevalence of 33% to 55% for central sleep apnea
has been reported in the 3 major studies in patients
with CHF. Enhanced sensitivity of the ventilatory
response to carbon dioxide in patients with CHF with
central apnea was reported by Javaheri and colleagues.
Enhanced sensitivity to carbon dioxide destabilizes
breathing during sleep, making this an important pathological
factor in CHF.
During sleep, PaCO2 rises and becomes the most potent
stimulus for augmented breathing. When the PaCO2 falls
below the apneic threshold, driven by the hyperventilation,
sleep apnea follows. Apnea persists until PaCO2 rises
above the threshold required to stimulate the ventilatory
response. The result is periodic breathing with recurring
cycles of apnea and hyperventilation, namely, Cheyne-Stokes
respiration.
Once triggered, the pattern of alternating hyperventilation
and apnea is sustained by a combination of increased
ventilatory chemoreceptor drive, pulmonary congestion,
and apnea-induced hypoxia, which causes oscillation
in PaCO2 above and below the apneic threshold. Central
sleep apnea elicits chemical, neurohormonal, and hemodynamic
oscillations including apnea, hypoxia, and oscillation
in PaCO2, which provokes periodic elevation in the
sympathetic nervous system, and surges in blood pressure
and heart rate.
Lanfranchi and colleagues presented the prognostic
value of the Cheyne-Stokes respiration in patients
with NYHA class II-III heart failure. Multivariate
analysis revealed that the apnea hyperpulmonary index
(AHI) and left atrial size were the only independent
predictors of subsequent cardiac death.
Although nocturnal oxygenation therapy using continuous
positive air pressure (CPAP) has been employed recently
for the treatment of sleep apnea, the effects of more
convenient nocturnal home oxygen therapy (HOT) in
patients with CHF and central apnea has not been verified.
|
|
|
Thus, this group conducted a multi-center, open-label,
randomized control trial to evaluate the efficacy
of nocturnal HOT on SDB, oxygenation saturation, cardiac
function, neurohormonal factors, and quality of life
(QoL) assessed by the Specific Activity Scale in patients
with CHF and central sleep apnea. The cost-benefit
analysis was a substudy.
To assess the Specific Activity Scale (SAS), patients
were asked to specify whether or not the patient could
perform each type of activity without symptomatic
limitation, according to the SAS scale questionnaire
(Figure
1). Summarizing the questionnaire data, a given
number of metabolic cost (METs) was derived for each
patient for the self-perceived exercise tolerance.
The inclusion criteria for this study were stable
outpatients over 20 years of age, NYHA class II-III,
oxygen desaturation index (ODI) þ 5 dips/hour, and
a left ventricular ejection fraction (LVEF) <45%.
The control group received conventional therapy and
the HOT group received conventional therapy plus nocturnal
HOT via nasal cannulae (3 l/min) using an oxygen concentrator.
Follow-up was 12 weeks. Patients with predominant
obstructive sleep apnea were strictly excluded from
the study.
|
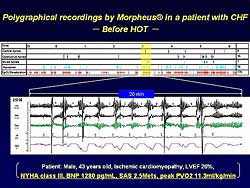 |
| Figure
3. Polygraphical recordings in a representative
patient before therapy nocturnal home oxygen therapy. |
| Click
to enlarge |
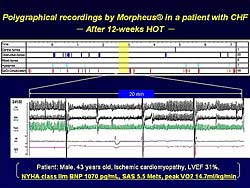 |
| Figure
4. Polygraphical recordings by in a representative
patient after nocturnal home oxygen therapy. |
| Click
to enlarge |
|
The baseline characteristics are shown in Figure
2. A total of 68 patients were enrolled from 20
centers and 56 patients were randomly assigned to
the 2 groups. There were no significant differences
in the baseline characteristics between the groups,
with respect to age, gender, sex distribution, underlying
heart disease, NYHA class, Specific Activity Scale,
medications, ODI or AHI.
In a representative patient, a 43-year-old male
with a 26% LVEF, NYHA class III heart failure, a BNP
level of 1280 pg/ml, and a 2.5 Mets SAS (Figure
3), Cheyne-Stokes respiration completely disappeared,
associated with stabilization of arterial oxygen concentration,
after 12 weeks of nocturnal HOT therapy (Figure
4). Further, the NYHA class improved to class
II moderate, BNP decreased to 1070 pg/ml, SAS increased
to 5.5 METs, and peak VO2 increased to 14.7 ml/kg/min.
Nocturnal HOT for 12 weeks, significantly improved
overnight arterial ODI from 9.5 dips/hour to 5.9 dips/hour,
and the AHI was reduced from 21 to 10 events per hour,
indicating stabilization of Cheyne-Stokes respiration.
In the control group, there was no significant change
during the study period.
The initial values of the SAS were nearly identical
in the 2 groups. Over the 12 weeks, a progressive
increase in the SAS score was seen in the nocturnal
HOT group, while it remained the same in the control
group. The between group difference was significant
at 12 weeks, indicating that HOT improved QoL, as
assessed by SAS.
Plasma ANP, BNP, and norepinephrine concentrations,
obtained every 4 weeks in the early morning, were
unchanged by 12 weeks of HOT therapy. No significant
change in PaCO2 was found. A significant improvement
in LVEF was found in the HOT group, while there was
no change in the control group (p=0.022). In summary,
the results of the main study showed that nocturnal
HOT stabilized Cheyne-Stokes respiration and arterial
oxygen. These improvements were associated with improvement
in cardiac function, LVEF, and QoL.
|
|
Cost-benefit analysis
The cost of illness was analyzed based on a questionnaire
survey of the morbidity in patients receiving nocturnal
HOT for more than a 6-month period, including the
study period. The reduction in cost of illness following
nocturnal HOT per year per patient was defined as
a benefit from treatment. The charge for the nocturnal
HOT was defined as a cost.
The survey questionnaire was sent to 33 physicians
at 20 institutions who participated in the present
nocturnal HOT study. The questionnaire asked about
frequency of hospitalization, emergency room visits,
and routine outpatient visits. The return rate for
the surveys was 85.3% and the data was collected regarding
53 patients.
After nocturnal HOT, the incidence of hospitalization
was remarkably reduced from 2.1 to 0.5 times per year,
a 76% reduction. The routine outpatient visits were
slightly reduced from 17.7 to 12.6 visits per year.
The emergency room visits were markedly reduced from
2.5 to 0.7 visits per year, a 72% reduction.
Medical costs were estimated using the database
of the central health insurance association in the
Ministry of Health and Welfare (February 2003). The
DPC MDC 5 diagnosis procedure combination charge for
the hospitalization due to heart failure was applied,
and the standard model case estimation for the emergency
room visit or routine outpatient visit.
Nocturnal HOT therapy was associated with a reduction
of 2 million yen in the cost of hospitalization over
1 year, a reduction of 15,000 yen in the cost of emergency
room visits over 1 year, and a reduction of 6,000
yen in routine outpatient visits over 1 year. The
cost/benefit per year was associated with a total
savings of 1,298,390 yen, including the cost of the
nocturnal HOT.
Because the cost of hospitalization is a major component
of the cost of treating CHF, a sensitivity analysis
based on the length of hospitalization was added.
The same database was used, which defined the average
hospital length of stay for uncomplicated heart failure
as 33 days for DPC MDC 5. The sensitivity analysis
revealed that a cost reduction with nocturnal HOT
is expected for hospitalization exceeding 16 days.
|
|
Conclusion
The present study demonstrated the clinical efficacy
and remarkable cost/benefit of nocturnal home oxygen
therapy as a novel non-pharmacologic treatment for
patients with CHF and central sleep apnea. The algorithm
for the treatment of the central sleep apnea-hypopnea
syndrome in heart failure should include maximizing
pharmaceutical therapy. In the setting of persistent
SDB, HOT or CPAP therapy should be considered or medications
such as theophylline or benzodiazepines. Heart transplantation
may be required in appropriate candidates.
|
PAGE
TOP
|
Interventional
Cardiology in the Elderly: Update of Non-Surgical
Interventions for the Treatment of Cardiac Failure
in Valvular Disease
Alain Cribier
Charles Nicolle Hospital, University
of Rouen, Rouen
|
|
Non-surgical interventional procedures offer new
therapeutic solutions to patients, mainly elderly,
for whom thoracic surgery is either declined or deemed
to be of high risk, because of fragility due to age
and comorbidities. Although the current gold standard
is thoracic surgery for either valvular repair or
replacement, today interventional cardiology plays
an important role for treating mitral valve disease
and mainly aortic stenosis.
|
|
Treatment of mitral stenosis
The metallic commissurotome is an instrument developed
by Cribier and colleagues about 8 years ago, as an
alternative to the treatment of mitral stenosis using
an Inoue balloon. The high cost of the Inoue balloon
technique is a problem in developing countries, especially
where there is a very high incidence of mitral stenosis.
Also, the Inoue balloon can create some mitral regurgitation
and some complication in patients with valves that
are very fibrotic and calcific.
The Inoue balloon is inflated in the center of the
valve and the commissure of the valve is opened by
traction. An alternative technique, mainly used in
the United States, is the double balloon technique,
which is more efficient to open the 2 commissures
with a direct effect. The metallic valulotome designed
by Cribier and colleagues has 2 metallic bars that
selectively open the valvular commissure. The efficiency
of the instrument to open very stiff, calcific, and
fibrotic valves is much higher. Double commissural
splitting is achieved in 86% of patients using the
metallic valulotome technique, compared to only about
30% with the Inoue balloon.
The detachable metallic head of the metallic valulotome
can be removed and reused up to 50 times, significantly
reducing the cost of the procedure. The commissurotome
is opened using hand-held pliers, up to a maximum
of 40 mm. The instrument is introduced trans-septally,
positioned in the middle of the valve, opened with
the hand-held pliers multiple times, with excellent
results. For example, the mitral valve area was increased
from 0.95 cm2 to 2.07 cm2 in
one patient.
A review of difficult cases in elderly patients
with very calcific valves showed that percutaneous
metallic commissurotomy was very successful. Overall,
in their experience, in young patients the achieved
MVA was 2.34 cm2, and in elderly patients
with calcific valves the MVA was 1.67 cm2,
exactly the same as achieved with the Inoue balloon
in a good population.
In their more than 4 years of experience in more
than 20,000 treated patients, they have demonstrated
the efficacy of the metallic commissurotome, that
complications are rare, and that there can be a major
economic impact.
|
|
Endovascular repair of mitral insufficiency
Mitral insufficiency is regularly treated by surgical
valve repair or replacement. Interventional cardiologists
have tried to develop some programs where mitral valve
repair could be done without the surgeon. This is
futuristic and the research programs are ongoing.
The percutaneous technique evaluated to treat mitral
regurgitation is a simulation of the Alfieri’s
surgical technique, which consists of stitching the
free edges of the mitral valve to create a double-outlet
on the mitral valve and reducing the mitral regurgitation
with 1 central stitch on the mitral leaflets. More
than 600 procedures have been reported since 1990.
For endovascular repair, interventional cardiologists
would like to use trans-septal access catheterization,
perforating the septum, catching the mitral valve,
and either stitching the valve or clipping the valve
using a special tool. In animal experiments, results
have been achieved that are exactly similar to that
achieved with the Alfieri’s surgical technique.
An alternative technique uses a nitinol clip (E valve)
that catches the 2 leaflets; the catheter is introduced
trans-septally.
Endovascular mitral repair using the coronary sinus
is also being researched. This involves using the
location of the coronary sinus in humans that is just
around the mitral orifice. The investigators imagine
the possibility of introducing inside the coronary
sinus a retractable annulus adjusted to remodel the
coronary sinus by narrowing the mitral valve annulus
to improve the coaptation of mitral valve leaflets.
In one experience, in 7 sheep, a 12 Fr sheath was
introduced via the jugular vein, and resulted in an
annulus diameter reduced from 2.55 cm to 1.83 cm (p=0.004).
At 6 months, there was a patent coronary sinus, patent
left circumflex, and no mitral regurgitation. It will
be some years before this can be performed in patients.
|
|
Percutaneous treatment of aortic stenosis
In elderly patients, the main concern is degenerative
calcific aortic stenosis. The best treatment for aortic
stenosis is aortic valve replacement, which is safe
even in old patients and can be done in the majority
of patients. However, many patients cannot undergo
surgery, especially patients with very old age or
comorbidities. Thus, balloon valvuloplasty and then
aortic valve replacement were developed.
Balloon aortic valvuloplasty is still performed
in many countries, and its use is increasing because
of the aging of the population. Despite the fact that
it is a palliative procedure, it can be re-done several
times and prolong the life of the patient by 5 to
6 years. The technique today is much simpler, carries
a low risk, and is much more efficient. Also, today
the limits of balloon valvuloplasty are known, which
are the usual persistence of significant stenosis,
and the limit of increasing the aortic valve area
above 0.8 cm2. So, the patients are left
with some aortic stenosis. The high mid-term restenosis
rate, which is unpredictable, can reach 80% at 1 year.
However, the functional status of the patient may
be improved after 1 year, despite the restenosis.
Yet, all patients are told the procedure will have
to be done again on average after 1.5 years.
The principle of balloon aortic valvuloplasty is
to break the calcium in the very calcific valves by
balloon inflation. The indications for balloon aortic
valvuloplasty are elderly patients (mean age 84 years),
with a very high surgical risk due to severely depressed
left ventricular (LV) function or comorbidities, patients
with major myocardial dysfunction (including cardiogenic
shock) as an attempt to improve LV function before
valve replacement (bridge to surgery), patients who
need urgent surgery for noncardiac reasons, and repeat
balloon aortic valvuloplasty for symptomatic restenosis
(up to 4-5 times).
In their experience in 148 consecutive patients
over 84years of age, death occurred in 4 patients
(mainly in patients with cardiogenic shock or very
poor LV function), stroke in 3 patients, ventricular
fibrillation in 1 patient, persistent atrioventricular
block in 2 patients, and surgical femoral complications
in 8 patients. The complication rate has been decreased
recently using a newer device.
|
|
Percutaneous heart valve implantation
The goal was to develop a biologic valve mounted
in a specific stent, which could be delivered percutaneously
via standard catheter-based techniques, within the
diseased aortic valve. The initial target population
is patients with severe calcific aortic stenosis who
are deemed inoperable or an unacceptable risk for
surgical valve replacement.
The last generation of the valve that is implanted
in man comprises a tricuspid valve made of equine
pericardium, which is sutured in a highly-resistant
stainless stent, with a maximal diameter of 23 mm.
It is delivered by inflating a balloon at 4 to 5 Atm,
a regular pressure for balloon inflation, and it can
be introduced with a 24 Fr sheath. The durability
of this valve in bench testing is more than 5 years,
satisfactory for the target population. The valve
is crimped, using a crimper device, over a regular
balloon, and introduced into a 24 Fr introducer without
any resistance.
The valve can be implanted via the antegrade trans-septal
approach or the retrograde approach via the femoral
artery. In the antegrade trans-septal approach, a
24-Fr sheath is introduced inside the femoral vein,
and the valve is introduced through the sheath. A
long guidewire is introduced from the femoral vein
and exiting from the femoral artery on the opposite
side, providing excellent support for the valve implantation.
The valve is positioned exactly where desired before
inflation, in the medium part of the calcium deposits
of the native valve leaflets. Accurate positioning
is extremely important. The aim is to have a stent
implanted at the exact site of the valvular calcification.
During balloon inflation, the heart is stimulated
at 220/min to block the flow and stabilize the balloon
during inflation. A super-aortic angiogram is performed
afterwards to observe the results. This procedure
is performed local anesthesia, with a procedure duration
of 90 minutes and 25 minutes of fluoroscopy time.
In the retrograde approach, a minimum diameter of
the femoral artery of 7 mm is required to introduce
the 24 Fr catheter. The procedure is performed under
local anesthesia, the duration is 60 minutes and fluoroscopy
time 20 minutes.
Procedural results include a reduction to nearly
zero in the mean gradient and a homogenous increase
in the aortic valve area to 1.69 cm2.
|
|
Conclusion
Percutaneous interventions bring new and promising
therapeutic alternatives for a large subset of patients
with valvular disease and cardiac failure, who are
too high risk or contraindicated for heavy thoracic
surgery. The development of percutaneous valve implantation
is particularly expected because of the increasing
incidence of degenerative aortic stenosis in the aging
population.
|
PAGE
TOP
|
Report
Index | Previous Report
| Next Report
Scientific
Sessions | Activities
| Publications
Index
Copyright © 2004
Japanese Circulation Society
All Rights Reserved.
webmaster@j-circ.or.jp
|
|