|
|
||||||
|
|||||||
|
|||||||
|
|||
|
|||
“Diastolic Dysfunction” in Heart Failure: Is it Time for a New Paradigm?Marvin A. KonstamTufts-New England Medical Center
|
Konstam proposed a shift in the view of diastolic heart failure and heart failure per se, including the terminology and categorization of patients. A new paradigm of heart failure and its characteristics should be considered, he stated.
The 3 most common characteristics of patients with heart failure (HF) in the United States, and quite likely in Japan, although the distributions within the countries may be different, are: ischemic, frequently referred to as having systolic dysfunction; hypertensive, frequently referred to as having diastolic dysfunction; and idiopathic dilated. However, gross structural abnormalities exist in each of these. The principal difference is that remodeling with enlargement and dilatation have occurred in the ischemic and idiopathic dilated hearts, while the hypertensive heart has remodeled with concentric hypertrophy and no enlargement of the cavity. Each of these hearts have similar characteristics; all are characterized by myocyte hypertrophy and by increases in interstitial collagen.
Further, the myocardium of these hearts is similarly abnormal, in that myocardial contractility of the individual myocytes may be abnormal, and diastolic properties of the myocardium are also abnormal.
Thus, categorizing cardiomyopathic hearts on the basis of their remodeling, that is, hearts remodeled with and without dilatation, was suggested by Konstam.
End diastolic volume drives differences in EF
Remodeling of a heart without dilatation is referred to as diastolic dysfunction and remodeling with dilatation is referred to as systolic dysfunction, in the setting of heart failure. Konstam suggests looking first at the end diastolic volumes, rather than the ejection fraction (EF), noting that the heart rate and the stroke volume are similar in the dilated and undilated hearts. Thus, it follows mathematically, that the smaller heart will have a larger ejection fraction and the bigger heart will have a lower ejection fraction.
That is further illustrated by a mathematical equation of the relationship between end diastolic volume and EF, under conditions of a constant heart rate and a constant cardiac index. In this fixed mathematical relationship, higher end diastolic volumes associated with low EF, and a lower end diastolic volume is associated with a higher EF.
In severe heart failure, for example, when the cardiac index falls to 2 L/min/m2, the curves shift slightly downward. Going from a cardiac index of 3 to a cardiac index of 2 at 200 ml/m2 is associated with a drop in EF only from 21% to 15%. End diastolic volume, not cardiac index, is actually driving differences in EF. Thus, for the most part, under the conditions of chronic, stable heart failure, EF is principally a derivative of whether the ventricle has or has not dilated.
Most of the patients with heart failure and preserved ejection fraction are elderly with long-standing hypertension with myocardial hypertrophy and fibrosis. In this population, in the setting of a non-dilated left ventricle (LV), compared to dilated cardiomopathy (DCM) with heart failure and a low EF, there are many similarities, including myocyte hypertrophy, interstitial fibrosis, abnormal calcium handling, reduced contractility, slowed relaxation, and depleted preload reserve. The principal difference between these conditions is the presence or absence of dilatation.
Characteristics of the syndrome of HF with preserved EF
The most common physiological characteristics in this syndrome are:
- abnormal relaxation
- abnormal compliance
- stiff vasculature
- abnormal renal function.
Abnormal relaxation. Gwathmy and colleagues showed that in the normal state, the cell handles calcium very effectively and removes calcium from the contractile elements and the cytoplasm very rapidly in early diastole, which is associated with rapid dissipation of early tension. In hypertrophic cardiomyopathy (HCM), in which there is abnormal diastolic performance, there is abnormal calcium handling, evidenced by a delay in calcium removal from the myocyte during diastole, associated with delayed dissipation of tension. In DCM with hypertrophic myocardium, there is severe derangement of calcium handling and delayed tension dissipation. Abnormality in calcium handling is generic in patients with heart failure, regardless of DCM or so-called diastolic dysfunction.
Abnormal compliance. The abnormality in compliance is thought to be mediated in part by increases in interstitial collagen. This has been well described in patients with HCM and in patients with DCM, who also may manifest increases in interstitial collagen. The increase in interstitial collagen results in abnormalities in diastole.
A small, but important study by Kitzman and colleagues studied 7 patients with HF with preserved EF and compared the relationship between LV end diastolic volume (LVEDD) and pulmonary capillary wedge pressure (PCWP) at rest and at exercise, and found that compared to normals, who were able to distend their LV and recruit preload with very little increase in PCWP, the patients with HF with preserved EF were unable to distend the LV and recruit preload, but PCWP increases dramatically, which is responsible for the elevation in wedge pressure and the inability to augment cardiac output during exercise.
A similar relationship was found in patients with HF and a low EF, in a study by Konstam and colleagues, looking at the ability of the LV to distend during exercise. The patients with no symptoms of HF during exercise have a distended LV at end diastole and therefore stroke volume is augmented. But the patients with symptoms of HF are characterized by higher stroke volumes at rest and an inability to distend the LV during exercise; an inability to recruit preload associated with an absence of a stroke volume contribution to the increase in cardiac output. So, patients with HF and a low EF are very clearly characterized by abnormalities in diastole, which may be load dependent and volume dependent, but, the abnormality in preload recruitment contributes to the reduced functional capacity.
Renal and vascular function in HF
The kidneys and the vasculature contribute importantly to the syndrome of HF. Konstam and colleagues showed in the SOLVD data that patients with lower calculated glomerular filtration rate (GFR), in patients with a very narrow range of serum creatinine, have a much worse prognosis than the patients with a more preserved renal function. These findings have been supported by many other investigators.
Two different studies showed a similar prevalence of renal dysfunction in patients with a low EF and a normal EF. This insufficiency is probably contributing to the overall syndrome of HF.
Pulse wave velocity, as an indicator of the vasculature, was shown to have an inverse correlation in patients with HF, that is, patients with stiffer vasculature have greater functional impairment, in a study by Bonapace and colleagues.
Patient characteristics in HF
The difference in gender distribution between the patients with HF and a low or preserved EF is the one distinct characteristic. Data from the Framingham Heart Study shows similarity in the characteristics of the patients with a low and normal EF in heart failure, including the frequency of hypertension (71% and 75%, respectively), age (74 and 72 years), coronary artery disease (72% and 57%), diabetes (22% ad 14%), and atrial fibrillation (36% and 35%). Gender is the major difference in the FHS data, with women comprising 25% of the patients with a low EF and 65% with a normal EF.
Heart failure with a preserved EF is typically more characteristic in the population, as shown in the series from the Mayo Clinic in their Olmstead County study data. However, if the distribution of age in patients with a low EF is simultaneously plotted with the data in patients with a preserved EF in this study, there are no striking differences.
Regarding prognosis, the data are mixed. In a study by Pernenkil and colleagues, mortality is lower in patients with a low EF compared to patients with a more preserved EF. However, a study by Senni and colleagues show a strikingly similar survival in patients with a low and more preserved EF. One difference may be that once patients begin to be admitted to the hospital with heart failure, the survival characteristics are not very different between patients with a low and preserved EF.
Treatment for patients with HF and preserved HF
In the patients with HF and a preserved EF in the CHARM study, the hazard ratio for the combined primary endpoint of cardiovascular death and hospitalization for heart failure was considered to be negative, because of the wide interval (HR 0.89; 0.77-1.02; p=0.118). However, Konstam considers this to show that angiotensin receptor blockers (ARBs) may be beneficial in these patients, especially when considering that the hazard ratios are not that different from the CHARM-Added arm (HR 0.85; range 0.75-0.95; p=0.011) and the CHARM-Alternative arm (HR 0.77; 0.62-0.9; p=0.118) of the trial. Also, some of the patients in the preserved EF arm may not have had much heart failure.
Trials are underway in heart failure with a normal EF, including:
- CHARM (candesartan vs placebo)
- PEP CHF (perindopril vs placebo)
- SENIORS (nebivolol vs placebo)
- HONG KONG (ramipril vs irbesartan vs placebo)
- PRESERVE (irbesartan vs placebo)
|
Data is also available from studies in “related” populations. The HOPE study with ramipril, the LIFE study with losartan, and the RENAAL study with losartan were not directed at patients with HF and preserved EF. However, each of the trials included patients with HF who have some very similar characteristics and in each case there was evidence of improved clinical outcome with either an ACE inhibitor or an ARB.
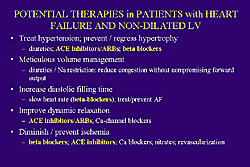
A rationale for treatment of patients with HF and non-dilated LV can be defined from a review of the treatment goals. These include the treatment of hypertension, volume management, increasing diastolic filling times, improving dynamic relaxation, and diminishing or preventing ischemia. Thus, treatment would include ACE inhibitors, ARBs, and beta blockers (Figure 1). The potential use of aldosterone blockade is very encouraging.
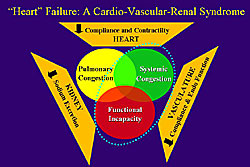
Rather than thinking about diastolic dysfunction and systolic dysfunction, Konstam recommends thinking about the hearts as being similar, and focus on the differences in dilatation in the LV. Konstam proposes thinking about this as a Cardio-Vascular-Renal (CVR) syndrome, rather than heart failure, where the heart, kidneys, and vasculature all contribute to the syndromes of pulmonary congestion, systemic congestion, and functional incapacity (Figure 2).
Conclusions
Heart failure is a clinical syndrome in which all patients have systolic and diastolic abnormalities. Left ventricles may be divided into dilated (low EF) and non-dilated (normal EF); the latter is common and mostly related to hypertensive C-V-R disease. Consideration might be made of adopting the term “Cardio-Vascular-Renal insufficiency”, which may be more appropriate than “heart failure”. ACE inhibitors or ARBs are indicated in the majority of patients. Patients with HF and left ventricles that are dilated and non-dilated should be enrolled in future trials of HF to determine whether important treatment differences exist.
|
|
| Copyright © 2005 Japanese Circulation Society All Rights Reserved. webmaster@j-circ.or.jp |