A New Method of Segmental Pulmonary Vein Antrum Isolation: Comparison of Efficiencies on Different Types of Atrial Fibrillation
Teiichi Yamane
Jikei University School of Medicine
Tokyo, Japan
|
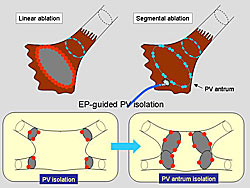
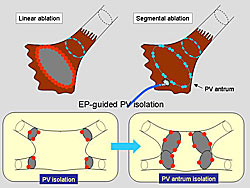
Figure 1. The new method used by Yamane and colleagues to target the antrum or left atrial posterior wall, which uses a larger-size Lasso catheter at the antrum for the EP-guided, segmental isolation.
Click to enlarge |
|
|
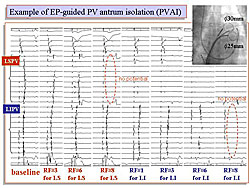
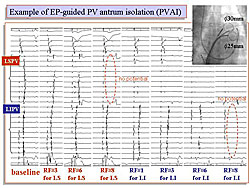
Figure 2. A typical example of the EP-Guided PV antrum isolation.
Click to enlarge |
|
|
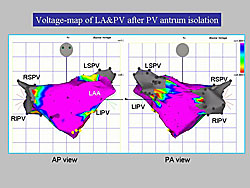
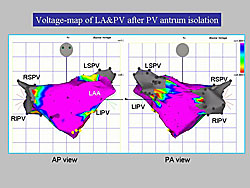
Figure 3. A voltage-map of the LA performed after the PV antrum isolation showed a scarred area without electrical activity in the PV and around their antrum. In the posterior wall, the scar area extended toward the LA midline from the contralateral ostium of the PVs.
Click to enlarge |
|
Isolation of both the pulmonary veins and their surrounding tissues from the left atrium (LA) is necessary for the effective treatment of atrial fibrillation (AF). Dr. Teiichi Yamane, Jikei University School of Medicine, presented results of a study comparing a new method of segmental pulmonary vein antrum isolation (PVAI) on different types of AF. The method used by Yamane and colleagues is shown in Figure 1.
Study patients underwent EP-guided segmental isolation of the PVAI with a large-size Lasso catheter (Figure 2). This method involved individual isolation of four pulmonary veins at the antrum. Segmental RF energy application was guided by a 20-pole, Lasso catheter of 25 or 30 mm diameter. Two Lasso catheters were positioned at the ipsilateral PV antrums. Ablation was performed with a deflectable catheter with an 8 mm tip. Power was applied at 30 to 35 watts with a temperature control of 50 to 55 degrees. The endpoint of ablation was bidirectional LA-PV conduction block at the antrum of each pulmonary vein.
A voltage map of the LA post-PVAI was performed to confirm the influence of ablation on the LA activation (Figure 3). A scarred area without electrical activity was observed not only in the PV itself but also around their antrum. In the posterior wall, the scar area extended toward the LA midline from the contralateral ostium of the PVs.
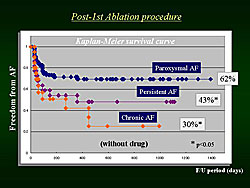
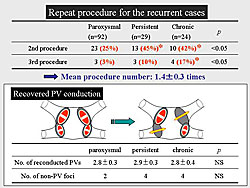
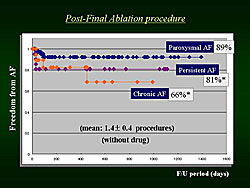
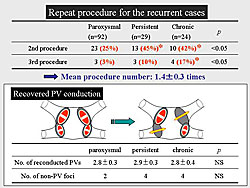
A total of 145 patients with AF were included in the study. Of these, 92 had paroxysmal AF, 29 had persistent AF, and 24 had chronic AF. All patients were followed for at least nine months after the procedure. After the first ablation procedure, 62% of patients with paroxysmal AF, 43% of patients with persistent AF, and 30% of patients with chronic AF were free of AF without taking drugs (Figure 4). A second procedure was performed in 25% of patients with paroxysmal AF, 45% of patients with persistent AF, and 42% of patients with chronic AF. A mean of 1.4 procedures were performed on each patient (Figure 5). After the final procedure, 89% of patients with paroxysmal AF, 81% of patients with persistent AF, and 66% of patients with chronic AF were free of AF, without taking drugs (Figure 6).
|
|
Figure 5. The results in the patients who underwent another ablation because of recurrent atrial fibrillation.
Click to enlarge |
|
Yamane concluded that EP-guided segmental PVAI using a large-size Lasso catheter is feasible, safe, and effective for treating AF. Recurrence of AF after the first procedure was more frequently observed in patients with persistent or chronic AF than in those with paroxysmal AF. However, repeat PVAI procedures targeting the reconducted pulmonary vein were shown to be equally effective in patients with all three types of AF. In the future, development of procedures for minimizing pulmonary vein reconduction and the systemic elimination of AF substrates in atrial tissues will be the next step in overcoming these arrhythmias. |