|
|
|
 |
Congress Report |
 |
the 70th Scientific Session |
 |
Symposia |
|
|
|
Pharmacological Intervention for CAD
|
|
|
|
|
|
α-Glucosidase Inhibitors are Protective Against Ischemia/Reperfusion Injury
Shinya Minatoguchi
Regeneration & Advanced Medical Sciences
Graduate School of Medicine, Gifu University
Gifu, Japan
Ischemic preconditioning protects the heart from infarction after a brief period of ischemia followed by reperfusion. Studies have shown that ischemic conditioning causes reduced glycogen utilization and myocardial lactate accumulation. Dr. Shinya Minatoguchi, Gifu University, presented results of two studies conducted to determine if pharmacological inhibition of glycogenolysis during ischemia provides cardioprotection.
Glycogenolysis is inhibited by α-glucosidase inhibitors. The α-glucosidase inhibitor, N-hydroxyethyl-1-deoxynojirimycin (miglitol), is a new antidiabetic drug that inhibits both α-1,4- and α-1,6-glucosidase. The effect of miglitol on myocardial infarct size was studied in rabbits subjected to 30 minutes of ischemia followed by 48 hours of reperfusion. The rabbits were treated with saline (control) or miglitol 1 mg/kg, 5 mg/kg, or 10 mg/kg. Rabbits that received 10 mg/kg miglitol had a marked reduction in infarct size compared to control rabbits, whereas the 5 mg/kg miglitol group had only a moderate reduction and the 1 mg/kg miglitol group had no reduction in infarct size. Miglitol also decreased the myocardial interstitial levels of 2,5-DHBA, an indicator of hydroxyl radicals; inhibited Bax protein expression; and decreased the incidence of TUNEL positive myocytes. Minatoguchi concluded that miglitol may be a breakthrough in the clinical application of ischemic preconditioning. Studies are needed to determine whether miglitol is beneficial for patients with coronary artery disease and diabetes mellitus.
The second study investigated the effect of the α-glucosidase inhibitor, acarbose, on myocardial infarct size in rabbits subjected to 30 minutes of ischemia and 48 hours of reperfusion. The rabbits were divided into five treatment groups: Control (no treatment), acarbose, acarbose + 5-HD (mitochondrial KATP channel blocker), sucrose, and sucrose + acarbose. Infarct size was significantly reduced in the acarbose and sucrose + acarbose groups compared to the control and sucrose groups. Infarct size was not reduced in rabbits treated with acarbose + 5-HD compared to control rabbits, showing that 5-HD blocked the effect of acarbose. Serum glucose levels of rabbits increased 60 minutes after being fed sucrose or placebo, but decreased after being fed acarbose or sucrose + acarbose. This study showed that oral administration of acarbose reduces myocardial infarct size via opening of the mitochondrial KATP channels. Improvement of postprandial hyperglycemia also may contribute to the infarct size-reducing effect of acarbose.
Minatoguchi concluded that α-glucosidase inhibitors such as miglitol and acarbose may provide new insights into therapeutic strategies for diabetic patients with coronary heart disease. |
Acute Effect of Statin in Patients with Acute Myocardial Infarction-SAMIT (Atorvastatin in Acute Myocardial Infarction Trial)
Koichi Node
Saga University
Saga, Japan
Experimental studies have shown that pretreatment with a statin decreases myocardial infarct size, partly due to nitric oxide (NO) production. Dr. Koichi Node, Saga University, presented results of SAMIT, a study of the effect of prior administration of atorvastatin on vascular inflammation and myocardial damage after primary PCI in patients with acute myocardial infarction (AMI).
This prospective randomized trial included patients with AMI admitted to the hospital within 12 hours of onset of symptoms who were candidates for reperfusion therapy. Patients in the atorvastatin group (n=42; 35 men) received 40 mg atorvastatin immediately after diagnosis, followed by 10 mg atorvastatin daily until day 30. They also received aspirin. Patients in the control group (n=45; 31 men) received aspirin and conventional therapy, but were not allowed atorvastatin for the first 30 days following AMI. The primary endpoints were death and cardiovascular events. Secondary endpoints were infarct size, reperfusion injury, left ventricle function, and inflammatory, platelet activation, and oxidative stress markers. Platelet derived microparticles (PDMPs), a coagulation factor in membrane phospholipids, were measured. PDMPs are involved in activation of platelets, leukocytes, and vascular endothelial cells, and are elevated in patients with AMI.
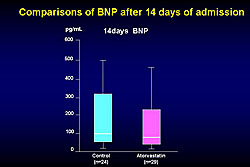
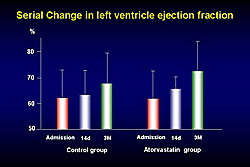
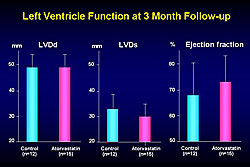
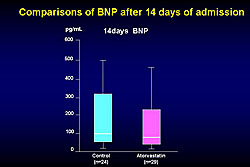
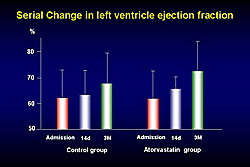
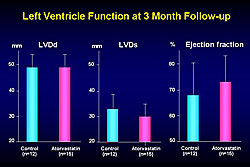
Baseline characteristics in both groups were similar, with a mean age of 61 in the atorvastatin group and 63 in the control group. Administration of atorvastatin attenuated the serial activation of PDMPs. There was a nonsignificant trend toward reduction in peak CPK in the atorvastatin group compared to the control group at 12 hours after admission. BNP was lower 14 days after admission in the atorvastatin group, but the difference was not statistically significant (Figure 1). Left ventricle systolic diameter (LVDs) decreased over time in the atorvastatin group compared with the control group, but not significantly. Left ventricle ejection fraction showed greater improvement over time in the atorvastatin group compared to the control group (Figure 2). At three months follow-up, left ventricle diastolic diameter (LVDd) was about the same in both groups, LVDs was lower in the atorvastatin group, and ejection fraction was higher in the atorvastatin group (Figure 3).
|
Figure 1. BNP levels after 14 days of admission in the SAMIT trial.
Click to enlarge |
|
|
Figure 2. Serial change in left ventricle ejection fraction in the SAMIT trial.
Click to enlarge |
|
|
Figure 3. Left ventricle function at 3 month follow-up in the SAMIT trial.
Click to enlarge |
|
These results showed a tendency toward reduced myocardial reperfusion injury, reduced BNP level, and improved cardiac function with atorvastatin treatment before PCI. Early administration of atorvastatin in patients with AMI might inhibit platelet activation and inflammation in the acute phase and may reduce myocardial reperfusion injury. Larger scale studies with longer follow-up are needed before definitive conclusions can be made. |
Effects of Early Statin Treatment on Symptomatic Heart Failure and Ischemic Events after Acute Myocardial Infarction in Japanese (The MUSASHI-AMI)
Tomohiro Sakamoto
Kumamoto University
Kumamoto, Japan
Lipid-lowering therapy with statins is associated with improved long-term survival in patients with coronary artery disease. However, few studies have investigated the effect of statin therapy during hospitalization for acute myocardial infarction (AMI) in Japanese patients. The MUSASHI-AMI trial, reported by Dr. Tomohiro Sakamoto, Kumamoto University, evaluated the impact of statin treatment initiated within 96 hours after the onset of AMI in Japanese patients.
|
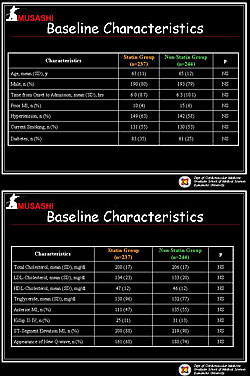
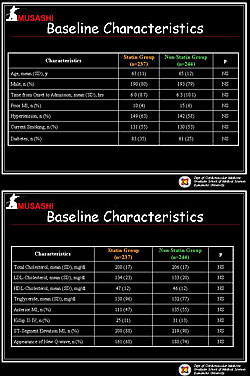
Figure 1. The baseline characteristics of the patients in the MUSASHI-AMI Study.
Click to enlarge |
|
|
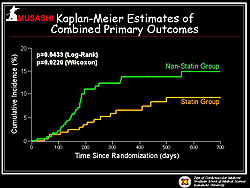
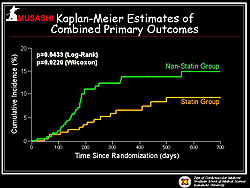
Figure 2. The combined primary results in the MUSASHI-AMI study.
Click to enlarge |
|
|
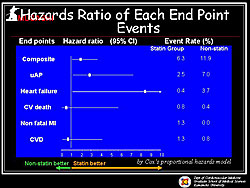
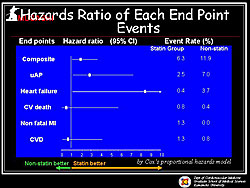
Figure 3. The hazard ratios for the endpoints in the MUSASHI-AMI study.
Click to enlarge |
|
|
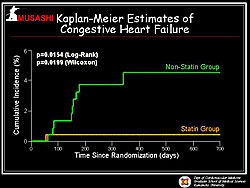
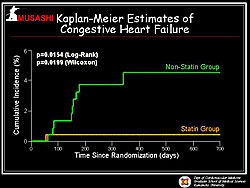
Figure 4. The Kaplan-Meier estimates of heart failure in the MUSASHI-AMI study.
Click to enlarge |
|
This prospective, randomized, open, blinded-endpoint trial enrolled 486 patients admitted for AMI with cholesterol levels from 180 to 240 mg/dL. Patients were stratified by center and randomly assigned to receive standard treatment with (n=241) or without (n=245) a statin and were followed for 24 months. The primary endpoint was a composite of cardiovascular death, non-fatal AMI, recurrent symptomatic myocardial ischemia requiring rehospitalization, congestive heart failure (CHF) requiring rehospitalization, and non-fatal stroke.
A total of 407 patients completed the trial. Baseline characteristics were similar in the two groups (Figure 1). The mean time from symptom onset to hospital admission was 6.2 hours. There was ST elevation or new left bundle-branch block in 89% of patients. Percutaneous coronary intervention (PCI) was performed in 90% of patients.
Pravastatin was the most commonly used statin (45%), followed by atorvastatin (34.5%). LDL cholesterol declined from 134 to 103 mg/dL after 24 months of statin treatment. A total of 16 primary endpoint events occurred in the statin group (n=237) and 29 events occurred in the non-statin group (n=244). Kaplan-Meier estimates showed a significantly lower incidence of combined primary endpoint events in the statin group compared to the non-statin group (p=0.0433) (Figure 2). Cox proportional hazard analysis showed that risk for CHF and unstable angina were significantly lower in the statin group (Figure 3). Kaplan-Meier estimates showed that CHF incidence was strikingly lower in the statin group than in the non-statin group (p=0.0154) (Figure 4). Kaplan-Meier estimates also showed a significantly reduced cumulative incidence of angina in the statin group compared to the non-statin group (p=0.0264).
Sakamoto concluded that statin therapy reduced recurrent cardiovascular events, in particular, symptomatic CHF requiring rehospitalization. In Japanese patients with AMI who had average cholesterol levels, early statin treatment reduced the risk of recurrent cardiovascular events, particularly the onset of CHF. |
|