|
|
||||||
|
|||||||
|
|||||||
|
|||
|
|||
State of the Art: Cardiorenal Syndrome and Hypertensive Heart DiseaseCarmine ZoccaliDivision of Nephrology, Hypertension & Renal Transplantation Riuniti Hospital, Italian RepublicDr. Carmine Zoccali, Riuniti Hospital, Italian Republic, reviewed current knowledge of cardiorenal syndrome and presented recent data on two major emerging risk factors that may provide targets for intervention. Cardiovascular (CV) disease is the main cause of death in patients with end stage renal disease (ESRD), while in patients with heart failure, the risk of death is inversely related to creatinine clearance. When they overlap, these two major organ failures constitute cardiorenal syndrome. The known Framingham risk factors trigger cardiovascular and renal damage. Once established, renal damage is a strong multiplier of cardiovascular risk due to risk factors inherent to chronic kidney disease (CKD)—anemia and hyperphosphatemia.
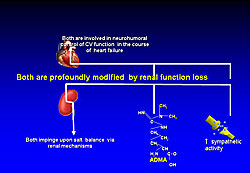
The three major emerging risk factors for cardiorenal syndrome are inflammation, high sympathetic activity, and accumulation of endogenous nitric oxide (NO) inhibitors. Dr. Zoccali focused on the latter two factors, both of which affect salt balance via renal mechanisms, are involved in neurohormonal control of CV function in heart failure, and are profoundly modified by loss of renal function (Figure 1). Sympathetic activity increases two-fold from normal in patients with mild to moderate CKD and even higher in those with ESRD. Asymptomatic ESRD patients with high sympathetic activity (norepinephrine [NE] >5.6 nmol/L) have a much higher risk of CV death (~45%) than those with NE <5.6 nmol/L (~25%). The risk of CV events is 90% higher in patients with high NE even after adjusting for other risk factors. In asymptomatic patients with systolic dysfunction, risk of CV death and heart failure is significantly higher in those with high NE levels. In the CAPRICORN study, treatment with the beta-blocker carvedilol reduced the risk of all cause mortality by 23% in patients with LV systolic dysfunction. In dialysis patients with dilative cardiomyopathy, carvedilol halved the risk of death.
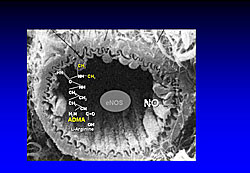
The endogenous NO inhibitor, asymmetric dimethyl arginine (ADMA) downregulates NO synthase (NOS) and NO production, which normally is stimulated by L-arginine (Figure 2). In a study of ESRD patients, Dr. Zoccali found that the risk of all cause mortality and fatal and non-fatal CV events increased with plasma increases in ADMA. Likewise, recent evidence in a large cohort of patients with heart disease showed that ADMA is a strong predictor of adverse outcomes. These studies provide convincing evidence that ADMA is a strong risk factor in ESRD and CHD patients. There have been few intervention studies in patients with CKD. Whether ADMA modification will improve CV outcomes in patients with compromised renal function remains to be tested, concluded Dr. Zoccali. |
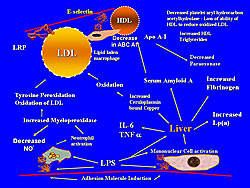
State of the Art: The Role of Inflammation and Dyslipidemia on Cardiovascular Risk in Patients with Renal DysfunctionGeorge A. KaysenUniversity of California Davis, Davis, USARenal failure is a powerful predictor of all cause mortality and cardiovascular (CV) events. In this presentation, Dr. George A. Kaysen, University of California Davis, discussed the risk factors for mortality and CV events in patients with impaired renal function. Risk factors among dialysis patients are different than those in the general population. In a study of 30,000 dialysis patients, the risk of death did not increase with increased serum cholesterol but in fact, increased significantly as cholesterol levels declined from the reference value. Analysis of lipoproteins in dialysis patients found increased VLDL and IDL but decreased LDL and HDL compared to controls. In the dialysis patients, increased VLDL, IDL, and LDL were associated with increased aortic pulse wave velocity. Distribution and structure of lipoproteins are altered in dialysis patients. The LDL fraction contains the more atherogenic small, dense LDL particles, which also have increased residence time, making them more susceptible to oxidation. The increased concentration of Apo B containing lipoproteins is due decreased clearance. As GFR declines, the levels of high molecular weight isoforms of Lp(a) increase, which is associated with increased CV risk.
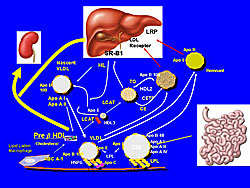
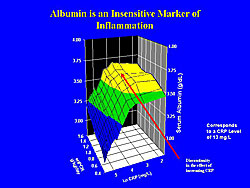
HDL and Apo A-I levels are reduced in ESRD patients. In one study, dialysis patients had 102 mg/dL Apo A-1 compared to 163 mg/dL in controls (p<0.0005). The mechanism of HDL reduction is increased clearance of small dense immature pre ß1-HDL (Figure 1). Low HDL levels are associated with mortality and incident vascular disease in patients with kidney disease. Hypoalbuminemia is the most powerful risk factor for death in dialysis patients, which has been attributed to malnutrition. However, increased C-reactive protein (CRP) is similarly associated with decreased survival. Further, when CRP was put into the model, albumin ceased to predict mortality (Figure 2). Hypoalbuminemia, as an independent predictor of CV mortality is primarily caused by inflammation. Patients with low albumin had high CRP values. The median CRP in dialysis patients is 8 mg/L, while the upper tertile in the general population is 3 mg/L, demonstrating a much higher level of inflammation in dialysis patients. Pro-inflammatory cytokine levels are also increased in dialysis patients, particularly IL-1, IL-6, and TNF-α. As cystatin-C levels increase, inflammatory cytokine, CRP, and fibrinogen levels increase. Additionally, serum amyloid A (SAA), also increased in dialysis patients, alters HDL structure and function. In summary, inflammation and dyslipidemia in patients with kidney disease are associated with subsequent altered vascular structure and an increased risk of CV events (Figure 3). |
Roles of Anemia and Erythropoietin in the Development of Heart Failure: Important Aspects of Cardiorenal SyndromeYutaka KagayaDepartment of Cardiovascular Medicine, Tohoku University Graduate School of Medicine, Sendai, JapanChronic kidney disease (CKD) and anemia both predict increased risk of death in patients with chronic heart failure (CHF). Potential causes of anemia in patients with CHF include renal angiotensin system (RAS) inhibition, proinflammatory cytokines, and CKD, which decrease renal secretion of erythropoietin (Epo) and bone marrow response to Epo. Dr. Yutaka Kagaya, Tohoku University Graduate School of Medicine, reported the results of two studies of the roles of anemia and Epo in development of CHF.
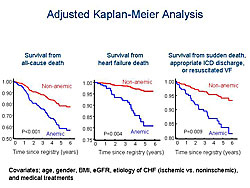
Dr. Kagaya and colleagues prospectively studied 365 stable patients with stage C/D CHF with LVEF ≥50% for a mean follow-up 3.7 years. Hemodialysis patients were excluded. Anemia was found in 42% of patients. Patients with anemia had lower eGFR, higher BNP level, and were less frequently treated with beta blockers. Kaplan-Meier analysis showed that CHF patients with anemia had significantly lower survival rates, taking into account all-cause death (p<0.001), heart failure death (p=0.004), and sudden death, appropriate ICD discharge, or resuscitated ventricular fibrillation (VF) (p=0.009) (Figure 1). These results suggest that anemia plays a crucial role in all-cause death, heart failure death, and sudden death, even in CHF patients with preserved LV systolic function. The second study was designed to determine whether endogenous Epo-mediated signaling protects against CHF and whether such beneficial effects are due to maintenance of hemoglobin or to its direct effects on the heart. The effects of LV pressure overload were studied in transgenic EpoR null rescued mice expressing EpoR mRNA only in hematopoietic cells. The EpoR-/- rescued mice and WT mice were subjected to transverse aortic constriction (TAC) or a sham operation. After one week, hematocrit was comparable in all four groups. LV weight and wet lung weight were significantly higher after TAC in EpoR-/- rescued mice compared with WT mice (p<0.05). LV diameter was increased (p<0.05) and LV fractional shortening was reduced (p<0.05) in EpoR-/- rescued mice after TAC compared to the other groups. The survival rate after TAC was 69% in EpoR-/- rescued mice compared to 90% in WT mice (p=0.004). VEGF expression was significantly increased only in WT mice with TAC, but not in EpoR-/- rescued mice with TAC, compared to corresponding sham-operated mice (p<0.01). Coronary angiogenesis was significantly increased in WT mice after TAC but not in EpoR-/- rescued mice (p<0.01).
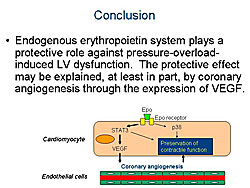
Dr. Kagaya concluded that the endogenous erythropoietin system protects against pressure-overload induced LV dysfunction. The protective effect may be explained, at least in part, by coronary angiogenesis through the expression of VEGF (Figure 2). These results suggest that both anemia and Epo signaling in the heart have important roles in development of heart failure. The Epo-EpoR system in the heart may be a therapeutic target in patients with CKD who have down-regulated endogenous Epo-EpoR signaling. |
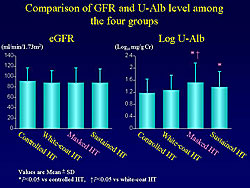
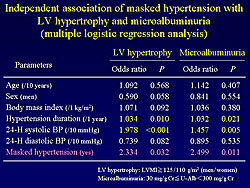
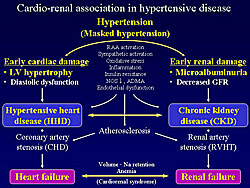
Cardio-Renal Association in Target Organ Damage of Hypertensive Patients: Involvement of Masked HypertensionTakeshi HorioDivision of Hypertension and Nephrology, Department of Medicine, National Cardiovascular Center, Suita, JapanDecreased GFR and microalbuminuria are predictors of cardiovascular events and death. Two studies, performed by Dr. Takeshi Horio, National Cardiovascular Center, Suita, Japan, and co-investigators investigated the association of these two risk factors with hypertensive cardiac changes and the influence of masked hypertension on cardiac and renal changes. A total of 475 non-diabetic patients with treated essential hypertension were enrolled in the first study. Patients with renal insufficiency or macroalbuminuria were excluded. Patients were evaluated by echocardiography for LV hypertrophy and diastolic function. Patients with normal GFR (eGFR ≥90 mL/min/1.73 m2) and low GFR (eGFR <90 mL/min/1.73 m2) had no differences in left ventricular mass index (LVMI) and relative wall thickness (RWT). However, patients with low GFR had decreased peak velocity ratio of early diastolic to atrial filling (E/A) (p<0.001) and prolonged deceleration time of the E wave (DcT) compared to those with normal GFR (p<0.001). Multiple regression analysis showed that eGFR was not independently associated with E/A and DcT. Patients with microalbuminuria (urinary albumin [U-Alb] ≥30-299 mg/g Cr) had increased LVMI (p<0.01) and RWT (p<0.05), decreased E/A (p<0.01), and prolonged DcT (p<0.01) compared to patients with normal U-Alb (U-Alb <30 mg/g Cr). Multiple regression analysis showed that the association of U-Alb with LVMI was statistically significant. Masked hypertension is associated with increased incidence of cardiovascular events when compared with controlled hypertension, white-coat hypertension, and uncontrolled hypertension. The second study examined the influence of blood pressure (BP) variation on cardiac and renal changes. Ambulatory BP monitoring and echocardiography were performed in 279 patients with treated essential hypertension. The subjects were divided into four groups according to 24-hour systolic BP and office systolic BP: controlled hypertension, white-coat hypertension, masked hypertension, and sustained hypertension.
LVMI was increased in patients with masked hypertension versus the other three groups (p<0.05) and in patients with sustained hypertension versus controlled and white-coat hypertension (p<0.05). E/A ratio did not differ among the four groups. There was no difference in eGFR among the four groups. Log U-Alb levels were significantly increased in patients with masked hypertension versus those with controlled and white-coat hypertension (p<0.05) (Figure 1). Multiple regression analysis showed that masked hypertension was independently associated with LV hypertrophy and microalbuminuria (Figure 2). These results indicate the presence of a cardio-renal association in hypertensive target organ damage and suggest that masked hypertension is a common independent risk factor for cardiac and renal damage (Figure 3).
|
|
|
|
Copyright © 2007 Japanese Circulation Society All Rights Reserved. webmaster@j-circ.or.jp |